According to Dr. Hong Zhi Jian, head of the external orthopedic department and leader of the research team on the project “Allograft on the Face” at the Nanjing Military General Hospital, China began clinical preparations and performed facial graft surgeries in 2003.
Preparing the “Materials” for Facial Grafting
In addition to the grafting process itself, the first challenge in facial transplantation is acquiring the “materials.” It is essential to obtain complete facial skin that includes sufficient subcutaneous fat, arteries, veins, and even nerves, while ensuring blood supply. Currently, this technique is fully achievable.
 |
|
Diagram of a facial graft surgery conducted by Chinese experts |
Dr. Hong Zhi Jian’s research team conducted cadaver studies to determine incision sites and layer separation, identifying which tissues under the skin could be removed, typically from the hairline down to the chin. During anatomical experiments, they discovered that if the neck skin was involved, it could compromise blood supply.
Among the various skin areas, the eyelid skin is the most challenging to work with due to its very small and thin structure, which is crucial for layered separation. If the eyelid skin is too thick after surgery, it may protrude, whereas if it is too thin, it may not ensure adequate blood supply.
The facial grafting technique requires the complete removal of the donor’s face within 6-8 hours post-mortem.
The team successfully harvested “materials” from a cadaver within half an hour, with additional time spent on cutting and refining the facial skin after retrieval. Since the skin can only tolerate a limited period of ischemia, the vascular connection must be completed within 10 hours.
In some other countries, animal facial grafting has been performed, such as grafting the facial skin of a black mouse onto a white mouse, where the white mouse’s fur continued to grow normally. However, these results are merely for reference, as human facial structure is unique.
After ensuring blood circulation, the challenge becomes restoring the facial expression capabilities.
Facial Reconstruction Post-Surgery
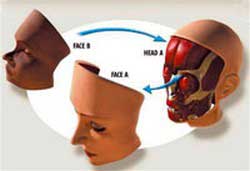 Initially, the level of facial deformation in the patient is assessed, followed by the viability of the grafted skin, ensuring that the donor skin and the remaining skin of the patient connect naturally.
Initially, the level of facial deformation in the patient is assessed, followed by the viability of the grafted skin, ensuring that the donor skin and the remaining skin of the patient connect naturally.
If the grafted facial skin is 5mm thick, after a successful procedure and waiting for inflammation to subside, it can return to normal thickness. If the newly viable skin is poorly integrated and swells to 15mm, deep muscle expression will be difficult due to reliance on muscle movement. If the surgery goes smoothly, basic expressions like smiling should not pose any issues.
Post-surgery, there may be a brief period where vascular obstruction causes skin necrosis, a common complication in microsurgery.
Moreover, the face is an external organ, making it susceptible to infections due to open wounds.
The greatest risk associated with facial grafting is postoperative rejection, a challenge that recipients will face for life.
In the days to 1-2 months following surgery, if acute rejection occurs, it can still be managed with medication. However, chronic rejection may not be effectively controlled by medication and can lead to necrosis and sloughing of the skin. Currently, this phenomenon can only be addressed at a level where, if the surgery fails, it can be corrected with conventional reconstructive surgery.
Rejection reactions will require lifelong immunosuppressant use, accompanied by potential side effects. At present, managing the side effects of these medications has only reached a safety level that does not endanger the patient’s life.
The new face after surgery will retain 60% of the patient’s original appearance and 40% of the donor’s features. For patients with typical burns, it is not advisable to undertake such a major surgery. This surgical method should only be applied to patients who have experienced serious accidents, severe burns, animal bites, or malignant tumors on the face.
Tuyet Nhung


















































