The cardiovascular complications of Covid-19 can lead to death if blood clots cause myocardial infarction, stroke, or pulmonary embolism.
Dr. Phan Thai Hao (Head of the Cardiology and Geriatrics Department at the Ho Chi Minh City Rehabilitation Hospital) stated that over 200 post-Covid-19 complications have been recorded worldwide across various organ systems. Respiratory, cardiovascular, neurological, and psychological complications are the most common, with cardiovascular complications being considered the most serious if not detected and treated promptly.
These complications can arise while the patient is still in the positive phase of nCoV, lasting several weeks or even months after the patient has cleared the virus. Initially, these injuries may not present obvious symptoms but can progress to serious cardiovascular diseases.
According to Dr. Nguyen Van Phuoc (Cardiology Department, Le Van Thinh Hospital, Ho Chi Minh City), the mechanism causing damage from Covid-19 is as follows: the virus binds to ACE2 receptors to enter cells. ACE2 receptors are most prevalent in respiratory endothelial cells, cardiac muscle, and vascular endothelium.
Damage to respiratory cells can lead to respiratory failure, potentially progressing to acute respiratory distress syndrome (ARDS). Damage to cardiac muscle cells can cause myocardial injury, myocarditis, and pericarditis. Notably, when the virus invades vascular endothelial cells, it attracts white blood cells, activates the inflammatory process, and releases cytokines and vasoactive substances. The destruction of endothelial cells exposes the subepithelial layer, causing vessel leakage and initiating the coagulation pathway. Because blood vessels are present in nearly all organs of the body, damage from Covid-19 results in multi-organ injury with various symptoms.
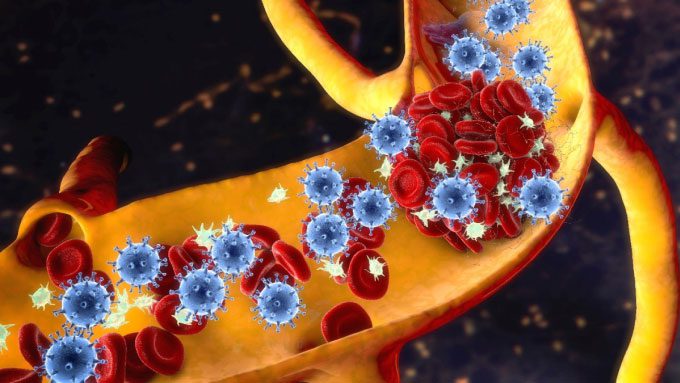
Blood clots can obstruct blood vessels, leading to many dangerous diseases. (Image: Shutterstock)
Cardiovascular complications can be categorized into two groups: those affecting the heart and those affecting blood vessels. Specifically, heart complications include myocardial infarction (due to blood supply-demand imbalance, coronary thrombosis); heart failure (occurring after myocardial infarction, in the context of the patient experiencing septic shock or ARDS); myocarditis, pericarditis (where the virus directly attacks cardiac cells), and hemothrombosis; Takotsubo syndrome due to stress (a type of cardiomyopathy).
Additionally, arrhythmias are common due to cardiac muscle damage, reduced blood oxygen levels, and electrolyte imbalances. Common manifestations include sinus tachycardia, atrial fibrillation, and bradycardia…
Vascular complications most commonly include hypercoagulation leading to thrombosis causing pulmonary embolism, deep vein thrombosis in the lower extremities, and cerebral infarction resulting in stroke. “These complications are very serious and can cause immediate death,” Dr. Phuoc stated.
Analyzing the coagulation complications post-Covid-19 in more detail, Dr. Hao noted three main causes leading to this condition. First, Covid-19 causes inflammation of blood vessel walls, disrupting coagulation, making the blood more viscous than normal. Second, patients with severe Covid-19 who are bedridden for long periods, are older, or have pre-existing chronic conditions (such as cancer, diabetes, hypertension, cardiovascular diseases, chronic lung diseases…) and are less active are more likely to experience blood stagnation.
The third, less common cause is individuals with special predispositions who lack one or more natural anticoagulant substances (such as protein C, protein S, antithrombin III, factor V Leiden…). Recently, Dr. Hao treated a pregnant woman who suffered a cerebral infarction due to a dual cause: complications from post-Covid-19 hypercoagulation and a deficiency in protein S. Although she has survived the acute phase, the patient must continue taking anticoagulants for an extended period to avoid the risk of recurrent stroke.
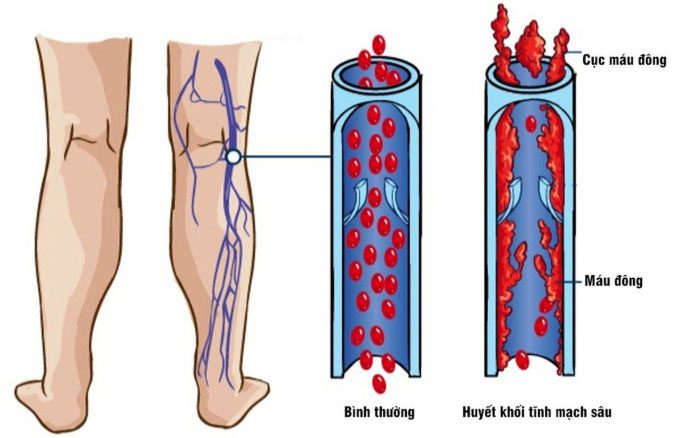
Simulation of venous thrombosis in the leg due to a blood clot. (Image: Amar Health)
In fact, in Ho Chi Minh City, many patients who recovered from Covid-19 months ago need to return for check-ups or even readmission due to cardiovascular complications. At Cho Ray Hospital, approximately 5-10% of patients visiting the post-Covid-19 clinic have coagulation complications. The post-Covid-19 cardiovascular clinic at Le Van Thinh Hospital also receives 3-5 similar cases daily.
A study from the United States published in Nature in October 2021 compared the risk of cardiovascular complications in over 151,000 veterans who survived nCoV infection with 3.6 million uninfected counterparts, noting an increased rate of heart attack, stroke, or cardiovascular complications in the first 12 months after recovering from Covid-19.
Specifically, non-hospitalized Covid-19 patients had a 39% higher risk of heart failure, and the risk of developing blood clots leading to pulmonary embolism increased 2.2 times in the following year compared to uninfected individuals. Thus, the world could see an additional 5.8 cases of heart failure and 2.8 cases of pulmonary embolism per 1,000 non-hospitalized Covid-19 patients. Among those hospitalized for Covid-19, the rate of cardiac arrest was 5.8 times higher, and the risk of myocarditis or pericarditis was 14 times higher. In patients admitted to intensive care units, these numbers were significantly higher. Nearly one in seven individuals suffered from some form of serious heart disease within a year after recovering from Covid-19.
To prevent worsening Covid-19 complications that affect health and quality of life, experts recommend that patients experiencing chest pain, shortness of breath, palpitations, leg swelling, difficulty breathing, or headaches should seek medical attention immediately for timely diagnosis and treatment. When signs of increased coagulation risk are detected, doctors will conduct additional blood tests, D-Dimer tests (to check for blood clots), and vascular ultrasounds to determine appropriate anticoagulant therapy. Typically, doctors prescribe anticoagulants for 5-10 days; if D-Dimer levels remain high, the patient will take anticoagulants for a month to minimize the risk of thrombosis.
Currently, many hospitals in Ho Chi Minh City, such as Le Van Thinh Hospital, Ho Chi Minh City Rehabilitation Hospital, Thong Nhat Hospital, Cho Ray Hospital, Xuyen A Hospital, and Ho Chi Minh City University of Medicine and Pharmacy, have opened specialized clinics for post-Covid-19 care or post-Covid-19 health check packages for the public.