Researchers at McMaster University have discovered a quick and effective way to “track down” cancer stem cells before the disease relapses in patients who have previously undergone treatment. Mick Bhatia, a professor in the Department of Biochemistry and Biomedical Sciences, led the new study, which was published in the journal Cell Reports Medicine.
Why Does Cancer Relapse?
Many cases of cancer recur in the body several years after prior treatment. Although current methods can monitor returning tumors, technology has not yet advanced enough to capture “undetectable” cancer cells. Bhatia’s research involving adults who have previously undergone treatment for acute myeloid leukemia (AML) marks a significant breakthrough.
Bhatia’s research involving individuals who have previously undergone treatment for acute myeloid leukemia (AML) marks a significant breakthrough.
Bhatia spoke about the promise of this new detection method and its implications for the future of cancer treatment.
What New Method Can Detect Cancer Stem Cells Before AML Returns?
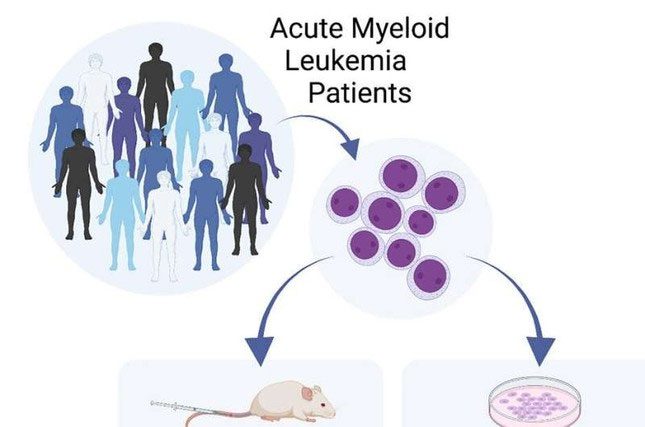
The detection method used by Bhatia’s team resembles the techniques employed to identify rare blood stem cells (progenitors) to assess the quality of cells donated for bone marrow transplants. This measurement has now been applied to AML patients, and they found that these progenitor cells carry specific gene mutations of an individual patient, which they call leukemia progenitor cells (LPC).
The detection of these LPCs can predict both short-term and long-term survival outcomes for patients, often outperforming previous measures used clinically or in laboratories to assess cancer stem cells (CSCs). This method has been successfully applied to a large patient sample of over 100 AML patients.
How Can This Method Be Applied in the Future to Other Types of Cancer, Including Solid Tumors?
For other types of leukemia, such as lymphoid leukemia, Bhatia’s team believes a similar progenitor testing approach could be utilized. They envision that this could also apply to solid tumors, but a new testing approach will be necessary since each tumor type is different. For example, breast tissue samples would be required to detect breast CSCs.
The team is excited about the prospect of solid tumor researchers using this “progenitor” model measured in vitro to predict patient outcomes, as they have established for AML in adults.
How Can Cancer Stem Cells Be Identified and Monitored to Lead to New or Modified Treatments, Ideally Before the Disease Relapses?
Currently, for AML, LPCs are measured using complex and expensive gene profiling or graft tests, where AML cells are injected into immunocompromised mice and measured over several months with multiple secondary assays required to assess these CSCs.
Bhatia’s team’s method could be easily and relatively inexpensively implemented in most laboratories, taking just eight days and costing only a few hundred dollars. This means that LPCs could even be measured during and after treatment to predict drug efficacy and the likelihood of cancer recurrence.
This would allow the research team to dynamically adjust treatment methods and monitor patients before the disease spirals out of control. This could improve patient outcomes by administering the best drugs based on LPC results at the right time during treatment.
If I or a loved one is a cancer patient, how can I detect cancer relapse?
Bhatia’s team can measure these rare cells that they believe are responsible for the recurrence of the disease—namely, cancer relapse. This would allow them to explore whether measuring these cells can help the team detect the disease, initiate earlier treatment, and/or modify treatment approaches during management to better eliminate these cells, with the hope of significantly improving survival rates and reducing harmful side effects of chemotherapy.
Ultimately, Bhatia’s research team is working on finding cheaper and faster ways to detect and understand CSCs, bringing them closer to developing therapies that target the root causes of cancer and reducing treatment times.


















































