According to new research, the injection of inactivated Staphylococcus aureus bacteria into tumors may stimulate first-responder cells to eliminate tumors in animal cancer models.
Introducing bacteria into the tumor microenvironment (TME) triggers an acute inflammatory response, which activates neutrophils—the first responders of the immune system—to attack the tumor.
This finding was published in a study led by the Garvan Institute of Medical Research in Australia.
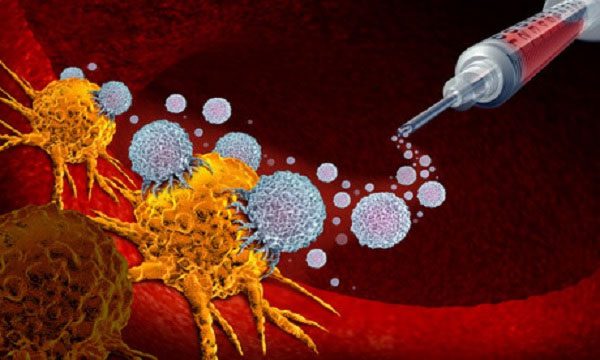
Injecting bacteria into tumors may stimulate neutrophils to eliminate tumors. (Image source: iStock).
The research published in the journal Cancer Research indicates that injecting inactivated Staphylococcus aureus bacteria into tumors can stimulate first-responder cells (neutrophils) to destroy tumors in animal cancer models, including Lewis lung carcinoma, triple-negative breast cancer, melanoma, and pancreatic cancer.
The study shows that most solid tumors produce a subacute inflammatory response, which supports TME in promoting tumor growth and inhibiting immune responses against tumors.
However, certain microbial formulations can shift the TME to an acute inflammatory response, helping to suppress cancer growth.
The researchers note that neutrophils typically function as a defense against diseases, but in some cases, they can also promote tumor growth, partly because they produce tumor-protective molecules and inhibit other parts of the immune system.
Ms. Tatyana Chtanova, a co-author of the study, stated that this type of neutrophil exists to attack foreign bacteria that invade the body.
Based on this principle, scientists have tested the idea of introducing bacteria into tumors to “attract” neutrophils to effectively destroy the tumors.
Additionally, the study found that neutrophils also change at the gene expression level, as they begin to secrete molecules that attract T cells—the second line of defense in the human immune system—for “reinforcements.”
Mr. Andrew Yam, another co-author of the study, assessed that the microbial therapy could enhance the effectiveness of checkpoint inhibition therapy (a type of immunotherapy for cancer treatment).
The researchers hope that this synergistic effect will create the best methods to improve treatment outcomes for patients with advanced cancer or previously untreatable conditions.
The research team plans to develop this therapy over the next 3-5 years for application in metastatic cancer stages, with clinical trials to be conducted.



















































