For women who frequently experience abdominal pain during menstruation, it may be worth considering the possibility of endometriosis. This is a benign condition that causes significant discomfort and pain for patients during each menstrual cycle. Additionally, it poses a risk of infertility in women.
What is Endometriosis?
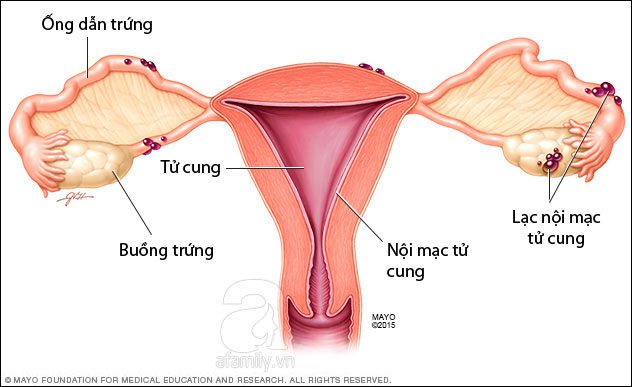
The endometrium is the mucous membrane that lines the uterus, situated on the surface of the uterus and separated from the uterine muscle layer. This mucous layer is influenced by estrogen during a woman’s menstrual cycle. Each month, if fertilization does not occur, the endometrial lining sheds and is expelled with menstrual blood. However, due to various reasons, fragments of this lining may flow backward into the fallopian tubes or even reach the ovaries. When these endometrial tissues exist outside the uterus, it is termed endometriosis. When blocked in areas outside the uterus, these fragments adhere to those locations and start to grow, causing inflammation and bleeding. In some cases, endometrial fragments can invade more distant areas within the abdominal cavity, such as around the intestines or bladder.
This condition is most common among women of reproductive age and is rare in postmenopausal women. The highest risk of developing this disease occurs between the ages of 30 and 40, although it can appear in girls as young as 8. According to statistics in the United States, an average of 6-10% of women are affected by endometriosis. In the UK, 1 in 10 women of reproductive age is experiencing this condition.
Causes of Endometriosis
The exact causes of this condition are still not clearly identified, but several factors have been mentioned. Various hypotheses, such as the mechanism of retrograde menstruation, congenital factors, and endometrial cell hyperplasia, have yet to be conclusively proven.
Endometriosis is common among women of reproductive age and rare in postmenopausal women.
- During menstruation, some blood may flow backward through the fallopian tubes into the abdominal cavity. The immune system in some women may react and produce immune responses. Normally, during menstruation, the uterus contracts gently from the body to the cervix to expel menstrual blood and detached endometrial tissue. However, in some individuals, there may be reverse contractions during menstruation, pushing menstrual blood backward into the fallopian tubes and abdominal cavity. This menstrual blood may contain “live” endometrial cells that have recently detached and are “traveling” throughout the abdominal cavity, where they stop and grow, also influenced by monthly estrogen, causing them to enlarge. Unlike when these cells are in the uterus, where they are expelled, in the abdominal cavity, they form cysts that do not detach but instead continue to grow. The more endometrial tissue present in the abdominal cavity, the more endometriosis lesions are formed.
- Thyroid issues can also increase the risk of endometriosis.
- Genetic factors can influence the likelihood of developing endometriosis. Research has shown that if a mother has endometriosis, her daughters are also at risk.
- Another possibility is that during the embryonic development stage, endometrial cells may dislodge from the uterus and migrate to surrounding organs.
- Endometriosis may also be influenced by environmental factors, although the exact mechanisms are still unknown.
- There’s a hypothesis suggesting that dormant cells in the body may suddenly develop into endometriosis lesions, or that remnants of primitive cells from the fallopian tubes may persist post-birth.
- During cesarean deliveries (which are common) or other interventions in the uterine cavity (gynecological procedures), the endometrial lining may fall into the abdominal cavity, leading to endometriosis.
Other causes may stem from immune system issues that prevent the body from recognizing and destroying endometrial tissues growing outside the uterus, resulting in endometriosis. Furthermore, you may develop the condition if abdominal and pelvic cells transform into endometrial cells, or if endometrial cells formed outside the uterus during fetal development persist.
Endometriosis commonly affects the entire fallopian tubes, ovaries, intestines, or tissues in the pelvic floor. The surrounding endometrial tissue can become irritated and painful, forming scar tissue and fluid-filled cysts, complicating conception.
Common Symptoms
The primary symptoms of the disease are pelvic pain, lower back pain, and lower abdominal pain. These pains may worsen during each menstrual period or during sexual intercourse. Additionally, symptoms like intestinal pain, bloating, and nausea during pain or digestive issues (diarrhea, constipation, indigestion) during menstruation are common signs of the condition.
Another typical symptom of endometriosis is menstrual irregularities, such as painful periods, prolonged cycles, and heavy bleeding. If you notice your menstrual cycle is unstable or that bleeding is unusually heavy, it is essential to consult a doctor for examination. Many women remain unaware of their condition until they encounter infertility issues.
Some common signs and symptoms of the disease include:
- Pelvic pain during menstruation that intensifies over time;
- Lower back and abdominal pain;
- Pain during or after sexual intercourse;
- Pain during bowel movements or urination during menstruation;
- Menstrual periods that may last longer or involve heavier bleeding;
- Blood in urine or feces, vaginal bleeding after intercourse;
- Fatigue, diarrhea, constipation, bloating, or nausea, especially during menstruation;
- Severe pain during menstruation;
- Pain before and during menstruation;
- Infertility;
- Fatigue;
- Some gastrointestinal disorders such as diarrhea, constipation, nausea.
Can Women with Endometriosis Get Pregnant?
Endometriosis leads to inflammation that can cause adhesions in the pelvic area, twisting or inflaming the fallopian tubes, which restricts or eliminates movement, preventing the capture of eggs released from the ovaries (known as ovulation).
When endometriosis occurs in the ovaries, it can damage ovarian tissue, naturally destroying follicles or causing inflammation and adhesion, thickening the ovaries and obstructing ovulation. Endometrial tissue within the fallopian tubes can make them less flexible, affecting the movement of sperm or eggs, and if significant, can block or occlude the fallopian tubes, leading to infertility. When endometrial tissue exists within the uterine wall, it alters the uterine environment, causing embryos (if the egg has been fertilized) to perish. Extensive inflammatory adhesions in the abdominal cavity can restrict or prevent the movement of the fallopian tubes.
Some factors that may lead to infertility due to endometriosis include:
- Very narrow fallopian tubes that are easily obstructed. Any blockage that hinders the egg’s transit along the fallopian tubes can result in infertility.
- Adhesions surrounding the tubes may prevent the movement of the egg along the fallopian tubes while also obstructing sperm from reaching the egg.
- Adhesions can displace the position of the fallopian tubes and ovaries within the pelvis.
- Endometrial tissue may cover the entire ovary, preventing the egg from being released into the fallopian tubes.
- When endometrial tissue appears in the uterus, it can cause bleeding. Similarly, when it is on the ovaries, menstruation will occur. If there’s no way to remove it, old blood may form cysts on the ovaries, affecting the ovulation process.
- Substances released due to pelvic inflammation may be detrimental to sperm and hinder the egg’s entry into the uterus. These substances can also adversely affect the endometrial cells, leading to problems during fertilization and early embryonic development.
- In some individuals, the ovulation process may be interrupted. If there are fewer eggs and ovulation is irregular, the likelihood of conception decreases.
- Endometriosis can reduce the quality of eggs as well as their potential for fertilization and development.
Only about one-third of women with endometriosis experience difficulties in conceiving. In reality, significant scarring and adhesions are typically required to impact fertility. Therefore, many women with endometriosis can still conceive normally. Some may receive a diagnosis after already having children. Nonetheless, endometriosis remains one of the leading causes of infertility among women. While some women may conceive, the success rate is not high because the growth of endometriosis lesions often correlates with time, while the chances of conceiving inversely relate to time. If the endometrial lesions are small and few (mild), the chances of pregnancy are higher; conversely, larger, more numerous, and adhesively affected lesions make conception more challenging.
Treatment and Prevention of Endometriosis
Currently, there is no definitive treatment for this condition. The available treatment methods are aimed solely at alleviating pain for patients and slowing the progression of endometriosis. Typically, individuals diagnosed with this condition are prescribed pain relievers or hormone-balancing medications, but these treatments cannot cure the disease and will lose effectiveness once discontinued. Additionally, patients may face various harmful side effects such as early menopause, vaginal dryness, and decreased bone density, leading to an increased risk of osteoporosis. In the most severe cases, patients may need to undergo laparoscopic surgery or a hysterectomy.
If the pain is unbearable, hormone therapy to reduce estrogen levels in the body can be employed to shrink the tissue. However, if you are planning to conceive, you may need to pursue fertility treatments and surgery simultaneously.
If you experience only mild pain, have no intention of becoming pregnant, or are approaching menopause, treatment may not be necessary. Medications such as hormonal contraceptives can be used to prevent the progression of endometriosis, or anti-inflammatory medications can help manage pain. If your pain becomes increasingly severe or the aforementioned medications and non-steroidal anti-inflammatory drugs are ineffective, stronger hormone therapy should be considered.
If stronger hormone therapy still proves ineffective or if other organs are affected, the next step is surgery. During surgery, large endometrial masses and scar tissue will be removed. These procedures will involve one or more laparoscopic surgeries, which remove endometrial cells and help separate adhesions from surrounding organs, returning them to their normal positions. However, surgery is not always effective, especially in severe cases. Some studies indicate that surgery may even reduce the chances of pregnancy.
During the removal of adhesions from the ovaries, there is a risk of mistakenly removing ovarian tissue. This not only affects future ovulation but also increases the risk of early menopause. The dissection of endometrial cells carries inherent risks, requiring high levels of expertise and precision. All surgeries come with complications, yet many individuals are willing to accept the risks to conceive and alleviate their pain.
A common treatment is the use of ovulation suppression medications. Oral contraceptives or combination hormone therapies containing progesterone can be prescribed.
Some individuals who have had enough children and find their lives significantly disrupted by endometriosis may opt for a hysterectomy. This is a last resort and should be carefully considered when symptoms severely impact daily life.
Preventive Measures for Endometriosis
- Regularly monitor your menstrual cycle: Pay attention to the regularity of timing, the volume of menstrual blood, and any pain experienced before and during menstruation. If your menstrual cycle is irregular, consult a doctor for evaluation.
- Maintain daily hygiene of the genital area to keep it clean and dry. Be cautious not to apply strong pressure deep inside the vagina to avoid the risk of bacteria penetrating and causing infections.
- Always maintain a healthy lifestyle and exercise regularly, particularly avoiding obesity. It is also advisable to steer clear of alcohol and stimulants such as caffeine. These measures help maintain a balance of estrogen, a hormone that stimulates the growth of endometrial cells.