Facial nerve palsy, or Bell’s palsy, is a common condition affecting individuals of all ages and genders, and it is not contagious. What causes this condition? Is facial nerve palsy dangerous, and how should it be treated correctly? Let’s explore these questions in the following article.
The facial nerve (Cranial Nerve VII) is responsible for motor control of facial muscles. Peripheral facial nerve palsy, also known as Bell’s palsy, is characterized by a complete or partial loss of movement in the muscles on one side of the face, due to damage to the facial nerve. This condition is distinct from central facial paralysis, which is related to brain injury.
Many are unaware that the facial nerve has a complex pathway from the central nervous system, passing through the temporal bone and the parotid gland to the facial muscles. This complexity explains why there are various causes of facial movement disorders, including issues arising from the brainstem, the facial nerve itself, the temporal bone, or the parotid gland.
Causes:
- Central VII nerve palsy: This typical facial paralysis is caused by lesions in the skull, leading to cerebrovascular accidents, tumors of the central nervous system, or acoustic neuromas.
- Peripheral VII nerve palsy: Damage to the VII nerve from the temporal bone outward, commonly known as Bell’s palsy, often results from cold exposure or inflammation.
How is Cranial Nerve VII Palsy Diagnosed?
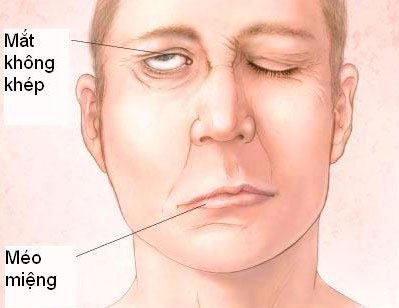
Peripheral facial palsy.
For cranial nerve VII palsy, diagnosis primarily relies on clinical signs. The physician will inquire specifically about the patient’s facial paralysis, identify the affected area, and determine the location of the damage based on the onset of facial paralysis and accompanying symptoms such as ear discharge, trauma, taste disturbances, and reduced tear production.
Additionally, the physician may diagnose the condition clinically by:
- Identifying peripheral facial paralysis with characteristic signs of damage, such as the Charles Bell phenomenon, where the patient cannot close their eyes completely.
- At rest, the patient’s face appears asymmetrical, with the affected side being pulled toward the unaffected side, forehead wrinkles are less pronounced compared to the opposite side, the eyebrow droops, and the mouth corner on the affected side is lower than the other side, with the cheek appearing slack and puffing out during exhalation.
- For closed injuries, the physician may observe differences in eyelash length when the patient tightly closes their eyes, with the lashes on the affected side being longer than those on the unaffected side.
In general, to accurately diagnose Cranial Nerve VII palsy, the treating physician must consider muscle tone at rest, examine the muscle groups in the face, and conduct other examinations such as:
- Ear examination: Look for blisters around the ear, ear discharge, and evaluate the tympanic membrane to help diagnose the underlying cause.
- Throat and neck examination: Palpate the neck and examine the throat to rule out parotid gland tumors.
- Neurological examination: Check for other associated cranial nerve injuries.
Patients exhibiting signs of Cranial Nerve VII palsy undergo clinical diagnosis, along with additional tests to accurately determine the condition and its causes.
- Magnetic resonance imaging (MRI) of the brain with cerebral vessels to identify whether the damage is central or peripheral.
- Other tests: Complete blood count, blood sugar, erythrocyte sedimentation rate, and biochemical tests…
Is Cranial Nerve VII Palsy Dangerous?
Cranial Nerve VII palsy can lead to various severe complications, including:
Ocular complications: These may include conjunctivitis, keratitis, corneal ulcers, and eyelid malposition. Such complications can be prevented by using protective eye drops, wearing glasses, or suturing the eyelid partially or completely.
Synkinesis: This is characterized by involuntary muscle contractions occurring simultaneously with voluntary actions, such as the mouth being pulled when closing the eyes. Failure to treat and rehabilitate can alleviate this discomfort.
Facial spasm after facial paralysis: This complication is seen in severe cases due to nerve damage with partial nerve reinnervation.
Sphenopalatine ganglioneuralgia: A rare condition that manifests as tearing while eating.
Treatment for Cranial Nerve VII Palsy
For Cranial Nerve VII palsy, physicians will implement medical treatment combined with surgical options to achieve rapid and comprehensive results for the patient. Depending on whether the condition is peripheral or central VII palsy, the treatment approach will vary:
- Peripheral VII palsy: The first step is to initiate medical treatment. Patients with Cranial Nerve VII palsy will be prescribed early, high-dose corticosteroids (1 mg prednisolone/kg) after ruling out contraindications (diabetes, tuberculosis, peptic ulcer, psychiatric disorders…)
Additionally, antiviral medications may be utilized in cases with viral infection symptoms or pain behind the ear, as well as sensory disturbances in the facial area. Surgical methods such as physical therapy, acupuncture, and facial exercises will provide comprehensive benefits for the patient.
- Central VII palsy: The underlying cause of the central damage must be identified, whether it be a tumor, infarction, or hemorrhage in the brainstem (where the nerve originates) to determine the appropriate treatment approach.
Be cautious: Facial paralysis can easily occur in winter and spring
Caution: Sudden facial paralysis and mouth drooping when the weather turns cold abruptly


















































