The body is a unified whole. The organs in the body work in coordination with each other. When one organ is diseased, it can affect one or more other organs to varying degrees. Oral diseases are no exception, as they are often related to many other health issues.
Gingivitis is a common oral disease. It causes bleeding, swelling, redness, and bad breath. Treatment includes proper oral hygiene and medication when the condition worsens.
1. Causes and Symptoms of Gingivitis
The primary cause of gingivitis is improper oral hygiene. This process leads to plaque buildup from food debris, saliva, calcium, and bacteria. Poor oral hygiene results in plaque accumulating around the gum line. When plaque penetrates too deep into the gum pockets, it creates periodontal pockets. These pockets harbor bacteria that cause gingivitis and root decay.
Some cases of gingivitis are not caused by plaque, but these are rare. Patients with weakened immune systems, such as those with diabetes, malnutrition, or cancer, are also more susceptible to gingivitis.
Hormonal changes during puberty, the menstrual cycle, pregnancy, menopause, or the use of oral contraceptives can also be risk factors that trigger gingivitis.
Common symptoms of gingivitis include redness, easy bleeding, bad breath, and discharge.
This condition needs to be treated early to avoid prolonged suffering and loss of confidence for the patient. If severe and left untreated, it can lead to periodontitis, dental abscesses, cavities, and ultimately tooth loss.

Gingivitis can lead to easy bleeding of the gums.
2. Treatment for Gingivitis
Since gingivitis is most commonly caused by improper oral hygiene, the first step is to ensure thorough oral care.
Oral Hygiene: Mild gingivitis can be effectively controlled and completely resolved through proper oral hygiene. In addition to regular dental cleanings every six months, daily brushing with a soft-bristled toothbrush is necessary to avoid damaging the gums. Patients with gingivitis may be advised to schedule professional cleanings every three months.
Use mouth rinses containing antibacterial agents such as chlorhexidine, hydrogen peroxide, hexetidine, zinc gluconate, or chlorine dioxide.
Medications for Treating Gingivitis: For more severe gingivitis, a doctor may prescribe specific medications:
- Antibiotics: Beta-lactam and macrolide antibiotics are first-line treatments that help eliminate bacteria residing in the gums. In cases of severe gingivitis leading to gum disease, periodontitis, or cavities, a doctor may prescribe a combination of macrolide antibiotics and metronidazole.
- Non-steroidal anti-inflammatory drugs (NSAIDs) (ibuprofen, diclofenac, meloxicam, etc.) are prescribed to reduce swelling and pain caused by gum inflammation. It is important to take these medications with food to avoid side effects.
- Pain relievers: Common pain relievers such as paracetamol are used to alleviate pain from gum inflammation.
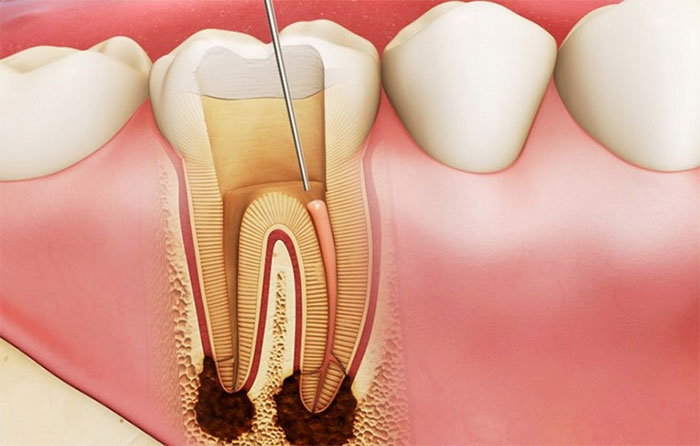
If gingivitis is not treated properly, it can lead to complications such as cavities and tooth loss.
In cases of hypertrophic gingivitis, a doctor may perform a procedure to remove excess gum tissue if necessary. If patients are taking medications that cause gum inflammation or hypertrophy (such as anticonvulsants, calcium channel blockers for hypertension, or immunosuppressants), these should be discontinued if possible. If discontinuation is not feasible, consider switching to alternative medications with similar effects.
Supportive Measures for Treating Gingivitis
In addition to medications and treatment measures for gingivitis, patients should pay attention to good gum care to facilitate faster healing.
- Use dental floss after each meal.
- Brush teeth twice daily with a soft-bristled toothbrush.
- Use antibacterial mouthwash.
- Maintain a balanced diet.
- Supplement with vitamin C through fruits such as grapefruit, citrus, strawberries, kiwi, papaya, and kale.
It is best to undergo a comprehensive health check-up to identify any underlying causes related to oral health. Remember to have dental check-ups and cleanings every six months. If you have cavities, they should be filled immediately.

















































