For centuries, humans have utilized honey for its antibacterial properties that have existed for millennia. Recent research has conducted numerous experiments demonstrating that Manuka honey can aid in the treatment of one of the most potent and drug-resistant lung infections, which is exceedingly difficult to treat.
Manuka honey originates from Australia, New Zealand, and Southeast Asia. It is named Manuka because this honey is produced by bees that pollinate the flowers of Leptospermum scoparium (commonly known as the Manuka bush).

Manuka honey originates from Australia, New Zealand, and Southeast Asia.
The flowers of the Manuka plant contain glycerone in their nectar, which, when converted into honey, reacts slowly to form methylglyoxal (MGO). This compound is unique to this type of honey and is not found in other varieties, and it is linked to its antibacterial properties.
Biologist Victoria Nolan states that utilizing a potential treatment method combining amikacin and Manuka honey holds promise as an improved therapy for severe lung infections.
Patients with pre-existing lung conditions, such as cystic fibrosis, are particularly vulnerable to Mycobacterium abscessus, which is distantly related to tuberculosis. Treating this bacterium is very complex, as some strains are resistant to various drugs. The treatment regimen includes 12 months of antibiotic chemotherapy alongside a variety of antibiotics, including amikacin, which can have severe side effects.
Even if patients can endure severe symptoms such as vomiting, potential hearing loss, liver damage, decreased white blood cells, and other blood coagulation-related components, the success rate of treatment remains a maximum of only 50%.
This aggressive bacterium can also cause persistent skin and soft tissue infections and can spread to any organ in our bodies.
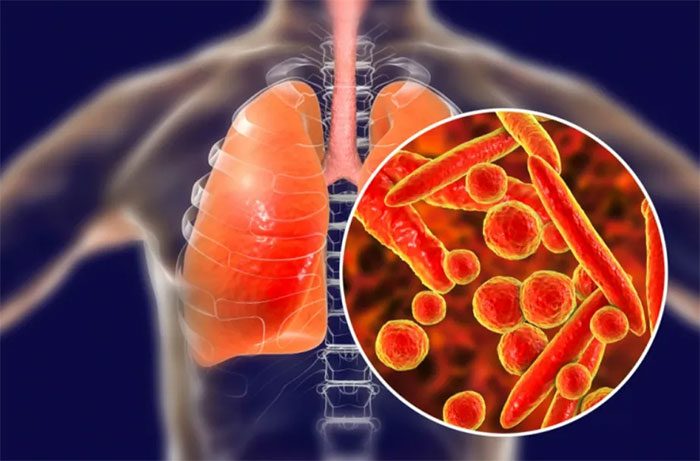
Drug-resistant lung infections are extremely difficult to treat.
A group of scientists tested various concentrations of this honey against bacteria in tissue cultures. They obtained strains of M. abscessus from 16 patients with cystic fibrosis or bronchiectasis, all of which were resistant to first-line antibiotic treatments. The results showed that all treatment methods involving Manuka could eliminate M. abscessus, with honey proving to be more effective than isolated MGO. This suggests that other active components in the honey may help counteract the bacteria’s drug resistance mechanisms.
The research team continued to experiment with a nebulized form of Manuka honey (a mist that can be inhaled) to be used alongside the antibiotic amikacin.
They found that the support from honey significantly reduced the amount of amikacin needed for treatment, decreasing the required dosage from 16 micrograms/ml to just 2 micrograms/ml. This would significantly reduce the dreadful side effects of the drug.
By combining a completely natural ingredient like Manuka honey with amikacin, one of the most important yet toxic drugs used to treat Mycobacterium abscessus, the experts have discovered a method capable of eradicating these bacteria with up to eight times less medication than previously required.
This has the potential to significantly reduce hearing loss caused by amikacin and greatly improve the quality of life for many patients.
The team also hopes that their discoveries will soon enter clinical trials. With over 100,000 people globally vulnerable to this pathogen due to cystic fibrosis, along with hundreds of thousands of others with bronchiectasis also at risk of infection, an effective treatment method like this is urgently needed, although it may not arrive soon enough.


















































