Blood type refers to the classification of blood, typically concerning the type of red blood cells. Our blood type can be completely different from that of our friends or even family members. Knowing your own blood type is crucial, especially for blood transfusions and medical purposes. This raises the question: why do humans have different blood types?
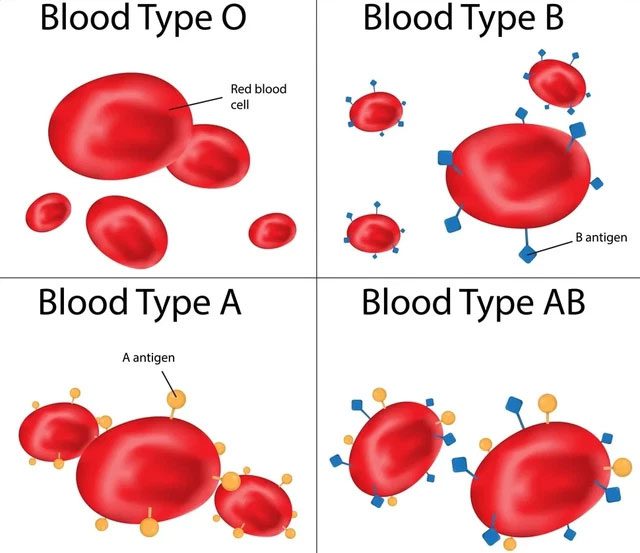
There are four main blood types in humans: A, B, AB, and O. Each blood type is determined by genetic antigens present on the surface of red blood cells. Blood type A has type A antigens on its red blood cells, blood type B has type B antigens, blood type AB has both A and B antigens, while blood type O has none. Typically, some antigens come from alleles of the same gene or are products encoded by closely linked genes, and these antigens form a blood group system. For humans, there are 30 different blood group systems identified and recognized by the International Society of Blood Transfusion.
Some studies suggest that the reason we have different blood types is due to malaria, and if you overlay a map of malaria parasites with a map of blood type O, you will find certain correlations between them.
Human blood is divided into various groups based on specific carbohydrates and proteins present on red blood cells. For reasons not yet fully understood, the blood of each group can have antibodies against the others. Therefore, when blood from a different group is transfused, the recipient’s antibodies can destroy the transfused blood, causing harm to the body.
Malaria causes a significant number of deaths each year. In 2020, approximately 627,000 people died from malaria worldwide. In individuals infected with malaria parasites, the infected red blood cells can accumulate in small blood vessels, obstructing blood and oxygen flow to the brain.
However, those with blood type O have a significant ability to resist malaria. A 2007 study showed that individuals with blood type O are 66% less likely to contract severe malaria compared to those with other blood types.
This occurs when the parasite invades red blood cells, expressing a family of repetitive interspersed proteins (RIFIN) on its surface. According to a 2015 study, RIFIN acts like glue, allowing uninfected red blood cells to cluster around the infected ones. At the same time, RIFIN binds strongly to the surface of type A red blood cells but weakly to type O red blood cells.
A blood sample can have over 30 substances on the surface of its red blood cells, and an individual’s blood type is one of the combinations of several blood group antigens. Among the more than 30 blood groups, over 600 different blood group antigens have been discovered, but most of them are very rare or primarily found in certain tribal groups.
However, blood type is not the only factor influencing a person’s risk of malaria. In addition to the antigens that make up the four main blood types, there are 15 other types of antigens that can appear on the surface of red blood cells, including a class of antigens known as Duffy antigens. Individuals lacking Duffy antigens have relatively strong resistance to one of the two major malaria parasites. In fact, the absence of Duffy antigens is relatively common in sub-Saharan Africa, where malaria is most severe, but rare in other parts of the world.
Scientists have found significant evidence to explain why people in malaria-prone regions tend to have blood type O. However, we still do not know why blood types A, B, and AB are relatively high in other areas. Some scientists have suggested that there may be a disease link between different blood types. For instance, individuals with blood type O are more susceptible to cholera, plague, tuberculosis, and mumps. Those with other blood types may be prone to different diseases; for example, individuals with blood type AB are more likely to contract smallpox, salmonella, and E. coli.
However, studies have yet to prove a causal relationship between blood type and the rates of these diseases, as other factors may contribute to the correlation. Therefore, these studies do not find evidence that blood type can protect against or predispose individuals to disease, and malaria is the only disease that is truly linked to blood type.

Currently, scientists do not know why most people’s blood cells have a type of protein called Rhesus factor (Rh factor) on their surface, making them Rh positive. About 15% of Caucasians, 8% of African Americans, and 1% of Asians lack this protein, resulting in their blood type being Rh negative (commonly denoted as + and – after the blood type, such as A+ or B-). Matching the Rh factor in blood types is crucial because mismatching during blood transfusions (transfusing Rh+ blood to someone with Rh- blood) can lead to dangerous complications. However, individuals with Rh+ blood do not experience issues when receiving Rh- blood.


















































