Japanese scientists have reported a case of “restless anal syndrome” following a Covid-19 infection, with initial examination results suggesting this syndrome in a man may be linked to SARS-CoV-2.
In a scientific paper published at the end of September in the BMC Infectious Diseases journal, the researchers noted that the patient, a 77-year-old man, experienced insomnia and anxiety when infected with SARS-CoV-2. Weeks after being discharged from the hospital, he began to feel restless and discomfort deep within the anal region.

Healthcare workers in protective gear caring for patients in the Coronavirus unit of Shaare Zedek Hospital in Jerusalem, Israel, on September 23, 2021. (Photo: YONATAN SINDEL / FLASH90)
The patient felt a desire to “move” in the anal area, and this sensation worsened during rest and in the evening. A colonoscopy revealed that the patient had internal hemorrhoids.
Restless anal syndrome is a form of restless legs syndrome (RLS). RLS has also been linked to some cases of Covid-19. However, this is the first report indicating a connection between restless anal syndrome and Covid-19.
The 77-year-old patient only experienced mild Covid-19 symptoms, being admitted to Tokyo Medical University Hospital with a sore throat, cough, and mild fever. He was treated for mild pneumonia, insomnia, and anxiety. Although the patient’s respiratory function returned to normal 21 days after hospitalization, insomnia and anxiety persisted.
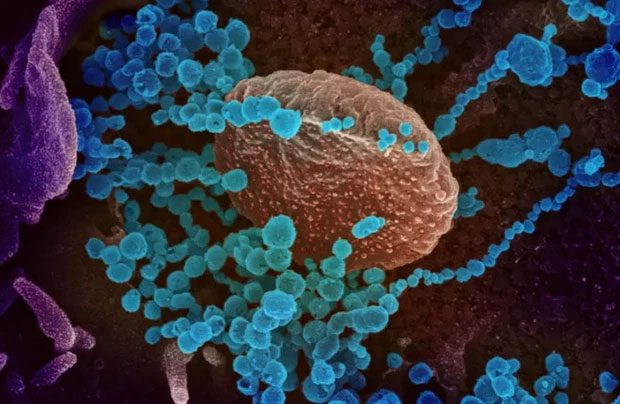
Microscopic image of the SARS-CoV-2 virus (Photo: U.S NIAID-RML / REUTERS)
Weeks after discharge, he began to feel discomfort in the anal area, a sensation he had never experienced before contracting Covid-19. Exercise alleviated the symptoms, while resting made the discomfort worse.
The scientists diagnosed the patient with restless anal syndrome after confirming that the symptoms matched the criteria and no other causes were found. They did not observe any signs of bladder or rectal issues or erectile dysfunction in the patient. Neurological tests showed no abnormalities, and the patient had no family history of RLS or periodic limb movement disorder.
The patient’s symptoms improved after being treated daily with 1.5mg of Clonazepam, a medication used for seizure disorders and panic disorders.
The scientists emphasized that the long-term neurological impacts of Covid-19 have yet to be fully understood, and it remains unclear how SARS-CoV-2 causes these effects. They called for long-term monitoring of these impacts to gain a better understanding of the underlying mechanisms. Additionally, they suggested that cases of RLS related to Covid-19 may not be adequately diagnosed.
Since mid-last year, researchers have identified several patients with mild Covid-19 who still suffer from neurological complications, such as encephalitis, delirium, nerve damage, and stroke.
|
SARS-CoV-2 may alter cell function When SARS-CoV-2 infects cells, it not only impairs cellular activity but can also change cell functions, according to a newly published study. For instance, when insulin-producing beta cells in the pancreas are infected with SARS-CoV-2, they not only produce significantly less insulin than normal but also begin to produce glucose and digestive enzymes—functions that are not characteristic of these cells. “We call this a change in cell fate,” said Dr. Shuibing Chen, the lead researcher from Weill Cornell Medicine in New York, USA. The study was published in the journal Cell Metabolism. The researchers noted in the journal that it is unclear whether these changes are permanent or reversible. Dr. Chen’s research team tested SARS-CoV-2 in organoids—clusters of cells that mimic internal organs such as the lungs, liver, intestines, and heart—but on a microscale. The study indicated that the loss of cell function could also occur in lung tissues, Dr. Chen told Reuters. |


















































