In just a few months, the Delta variant has overshadowed all other virus variants. At this point, Delta has become the dominant virus strain in the pandemic across nearly every continent in the world.
The rapid development and dominance of the Delta variant in the pandemic have raised concerns among scientists about the virus’s potential for mutation, along with the unforeseen consequences it may bring.
With billions of people still unvaccinated worldwide, the virus continues to have opportunities not only to spread but also to generate new mutations.
Some scientists hope that the virus has reached its peak evolutionary threshold, but there is no evidence to suggest that it will stop mutating.
Dangerous Breeding Grounds
More than one factor has contributed to the rise of the Delta variant. Human behavior is the primary reason. In many countries, the Delta variant surged and spread like wildfire after the number of infections had dropped to very low levels, in some places to zero.
As people returned to near-normal lives, restaurants, bars, nightclubs, and cinemas became crowded again, and people became lax about wearing masks and social distancing. This was when the Delta variant flared up, bringing the pandemic back in full force.
South Asia, East Asia, Western Europe, and now North America all share a similar scenario, with outbreaks occurring just when it seemed the pandemic was nearing its end. This time, the enemy is the Delta variant.

Florida beach crowded with tourists in early April. (Photo: Reuters).
The second reason is vaccination rates not meeting expectations. In wealthy countries where vaccines are abundant, a significant portion of the population still harbors anti-vaccine sentiments. Even in countries like the United States, Germany, France, and Italy, about 30% of the population has not been vaccinated.
In poorer countries, the obvious issue is the lack of sufficient vaccines. In East Asia, aside from Singapore and China, no country has achieved a vaccination rate of over 50% for at least one dose, not even in nations like Japan or South Korea.
The situation is even worse in Africa, where the number of vaccine doses administered accounts for less than 5% of the total vaccines used globally.
And the Delta variant itself is a particularly unique strain. The rapid global dominance of Delta is evidence that this variant is very different. Scientists are still conducting research to fully uncover the mysteries behind the differences of the Delta variant.
What worries scientists the most right now is that the coronavirus shows that the longer it exists and spreads among humans, the more dangerous it becomes.
The original strain of the virus that emerged in Wuhan had an R rate—meaning the infection rate—of about 2.5. This rate means that each infected person would transmit the virus to 2-3 other people.
An R rate greater than 1 indicates that the disease is spreading. The U.S. Centers for Disease Control and Prevention states that Delta has an infection rate greater than 5.
Increased Virulence?
Scientists are still unsure whether Delta is more virulent than older virus strains, as there is not enough evidence yet.
Stephen Brierre, head of the intensive care unit at Baton Rouge General Hospital in Louisiana, stated that respiratory symptoms leading to the need for ventilators in Delta-infected individuals appear earlier.
“From what we observe, they seem to deteriorate more quickly,” Brierre said.
Emily Tulle, a nurse at Willis-Knighton Medical Center in Louisiana, noted that she has witnessed more cases of kidney failure, liver failure, and blood clots since the Delta variant became the dominant strain in the U.S. The nurse mentioned that more patients require ventilators than before.
Previously, each nurse at Willis-Knighton was responsible for two patients in the intensive care unit. In recent weeks, “patients are so ill that they require one-on-one care,” Tulle said.

Inside the intensive care unit at Bergamo hospital, Lombardy, Italy. (Photo: Sky).
There are many young patients being hospitalized and dying in the current wave of the pandemic compared to before. This phenomenon is not unique to the United States but is being reported globally.
Data from healthcare facilities worldwide show that vaccination remains the most effective shield. Although there is still a risk of contracting the virus, vaccinated individuals are highly protected against severe illness or even death.
Epidemiologists hope that with a vaccination rate of 70-80%, combined with the number of people who have natural immunity due to previous infections, the pandemic can be controlled.
However, a variant like Delta, with a higher transmission capability, means that humanity will need to achieve a higher vaccination rate, around 90%.
Even in developed countries like the U.S., reaching 90% will not be easy due to the anti-vaccine mindset among a significant portion of the population. Globally, vaccination campaigns will take many years to achieve the desired rates.
P681R Mutation
Humanity has never been able to observe a virus evolving in detail as it can today. Advances in gene sequencing technology over the past few years allow scientists to track the virus’s changes in real-time, witnessing one strain evolve into another.
Scientists say that the mutations of the Delta variant, when viewed superficially, do not stand out compared to other variants it has outperformed. In fact, Delta lacks some mutations that help it evade the immune system, which were present in the Beta and Gamma variants.
However, on Delta, a mutation known as P681R has been identified, which may be key to this variant’s dominance.
The coronavirus enters human cells in two steps, similar to inserting a key into a lock before turning it to unlock.
Most mutations in other “variants of concern” seem to help the key fit better into the lock, according to Professor Vineet D. Menachery, a virus expert at the University of Texas.
However, the P681R mutation helps the key unlock more easily. This is why the Delta variant is very effective at penetrating human cells, Menachery stated.
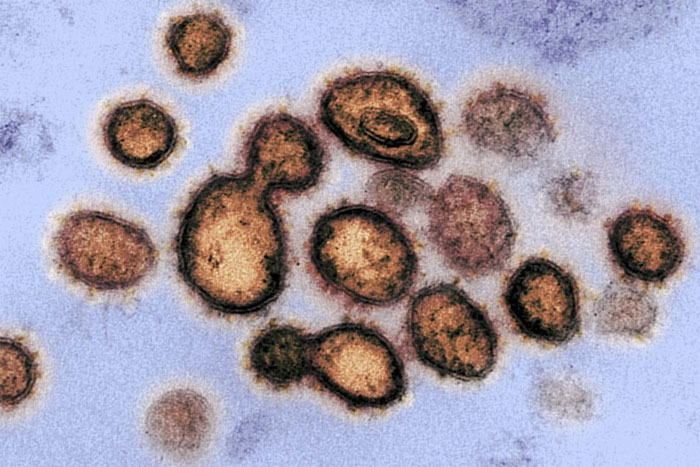
SARS-CoV-2 Virus. (Photo: Rawpixel).
Most research is currently focused on the spike protein, which helps the virus invade cells. However, Delta has mutations that affect other parts of the virus, and there has been limited research on the remaining altered components beyond the spike protein, as well as their effects on the human body.
Nevan Krogan, a scientist at the Gladstone Institute of Data Science and Biology, noted that the Alpha variant transmitted strongly due to its ability to suppress the natural immune response of humans, which is the first line of defense against the virus. Krogan and his colleagues are currently investigating whether the Delta variant has similar capabilities.
“When variants emerge, everyone talks about the spike protein. Clearly, the spike protein is involved; it helps the virus enter cells more easily, but there are also other mutations that somehow suppress the immune response,” said Mr. Krogan.
Professor Menachery describes the Delta variant as a “timely virus,” as it appeared and rose at the perfect moment for it to become the dominant strain.
The lingering question is whether Delta is the most perfect form of the SARS-CoV-2 virus or if it could still acquire additional mutations, making the virus even more formidable.
“Delta surprised me. I have never been surprised by the flu or Ebola,” said Trevor Bedford, a virus evolution expert at the Fred Hutchinson Research Center.
Mr. Bedford believes that the virus cannot continue to evolve indefinitely to become dangerously limitless. Ultimately, every organism has an evolutionary ceiling.
“But right now, we are unclear about what the evolutionary ceiling of the SARS-CoV-2 virus is,” Mr. Bedford stated.



















































