Leptospirosis is a contagious disease caused by the spiral-shaped bacterium Leptospira in humans and animals. In humans, this disease can cause a range of symptoms and can be fatal. In Vietnam, about 5% of patients have detected Leptospira in their serum. The Leptospira IgG/IgM test provides initial preliminary results, aiding in the diagnosis of leptospirosis.
Overview of Leptospirosis
What is Leptospira?
Bacteria (sometimes referred to as germs) are a group of unicellular prokaryotic microorganisms that are extremely small – visible only under a microscope – found everywhere including soil, water, air, and even as symbionts and parasites in other organisms. Leptospira refers to bacteria that have a spiral shape, commonly seen in pathogens such as those causing syphilis or yellow fever.
Leptospirosis is an infectious disease transmitted from animals to humans caused by the spiral-shaped bacterium Leptospira. Leptospirosis is a dangerous condition that can lead to systemic intoxication, hemorrhaging, liver and kidney failure, resulting in a high risk of death for affected individuals.
Causes of Leptospirosis
- Leptospira is present in the urine, blood, and internal organs of rodents, livestock, reptiles, and amphibians, with rats and rodents being the most significant hosts.
- Leptospira enters the human body through skin wounds, wet skin, mucous membranes of areas such as the nose and mouth, or by ingesting contaminated sources. Patients contract leptospirosis when organs such as the eyes, nose, mouth, or open wounds come into contact with urine, blood, secretions, or tissues of infected animals or through bites from infected animals.
- Additionally, individuals can become infected by coming into contact with contaminated water or soil harboring the bacteria.
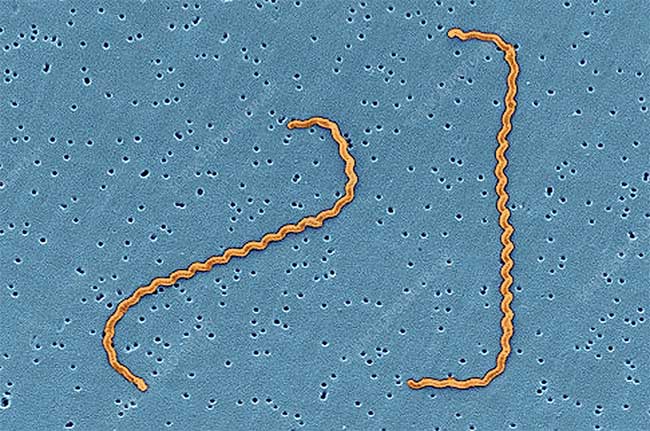
Image of Leptospira interrogans.
Symptoms of Leptospirosis
The symptoms of leptospirosis occur in two stages:
- Initial stage lasts from 5 to 7 days, starting suddenly with symptoms including: high fever, vomiting, diarrhea, muscle pain, chills, and headaches.
- Second stage may appear after 1 to 2 weeks with symptoms such as: jaundice characterized by yellowing of the skin and eyes, systemic intoxication, hemorrhage, liver and kidney failure, lung issues, irregular heartbeat, and meningitis.
Leptospirosis is very dangerous; if not diagnosed and treated promptly, it can lead to life-threatening complications.
At-risk groups for Leptospirosis
- Leptospirosis is a common disease affecting individuals of all ages. Some high-risk groups include those who work outdoors or frequently come into contact with animals, such as veterinarians, farmers, sewage workers, slaughterhouse employees, livestock traders, and miners.
- Leptospirosis is a disease that only transmits from animals or sources to humans and does not spread from person to person.
Prevention of Leptospirosis
- For livestock and poultry, it is important to vaccinate animals at risk fully to prevent the disease. Animal enclosures should be regularly checked and cleaned to ensure the health of livestock and isolation when illness occurs.
- For those in contact with animals: Protective measures should be taken when handling livestock, and there should be protocols for managing and isolating sick animals. Additionally, individuals should boost their immune systems through regular exercise, limiting alcohol consumption, and maintaining a balanced diet. If symptoms arise, seek specialized medical attention to confirm the disease and obtain the best treatment.
Diagnostic measures for Leptospirosis
The diagnosis of leptospirosis is based on clinical examination combined with diagnostic tests.
- A clinical examination checks for symptoms of leptospirosis. Doctors assess the patient’s symptoms to differentiate from other diseases such as dengue fever and provide appropriate testing and treatment recommendations.
- Blood tests to identify the cause of the disease help determine the infection and assess the progression of the disease, especially if acute complications have occurred.
- Blood culture and isolation of secretions from the patient to accurately identify the causative agent support the doctor’s diagnosis and enable timely and appropriate treatment.
- X-rays, ultrasounds, and other imaging techniques are employed to identify lesions and complications to correctly assess the patient’s condition for suitable treatment.
Treatment measures for Leptospirosis
Accurate identification of the cause through diagnostic measures helps doctors direct treatment effectively.
In most cases, leptospirosis is mild and resolves quickly. However, if patients are careless and underestimate the seriousness of their condition, the disease may progress to a dangerous stage, threatening their lives.
In severe cases, patients require close monitoring and aggressive treatment to prevent life-threatening developments. In such instances, doctors will use antibiotics as recommended and implement supportive measures to alleviate symptoms, such as intubation or dialysis. After treatment, patients should monitor recovery, rest, and receive nutritional support for swift healing.