According to the Centers for Disease Control and Prevention (CDC) in the United States, some outbreaks of the I strain of the monkeypox virus have resulted in a mortality rate of up to 10% among those infected.
On August 15, the World Health Organization (WHO) declared the ongoing monkeypox outbreak in Africa a global health emergency, the highest alert level under international health regulations. This announcement followed the declaration of a public health emergency made by the Africa Centers for Disease Control and Prevention for the continent on August 14.
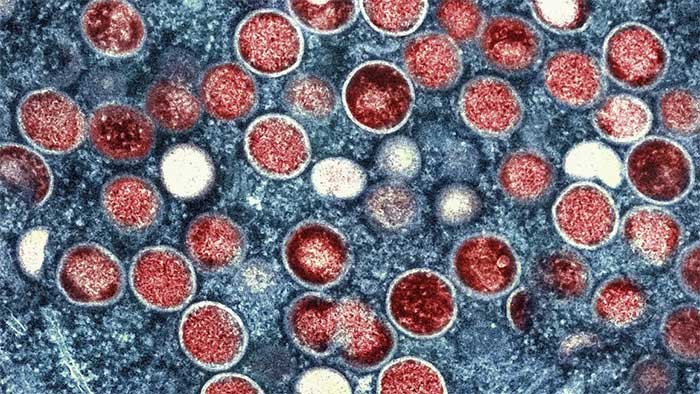
Monkeypox viruses found inside an infected cell. (Source: AP).
A more lethal strain, the Ib branch, is rapidly spreading in the Democratic Republic of the Congo and has reached at least four previously unaffected countries in Africa. WHO Director-General Tedros Adhanom Ghebreyesus stated that the risk of international spread is “very concerning.”
Dimie Ogoina, Chair of the WHO Emergency Committee, noted: “All agree that the current monkeypox outbreak is an unusual event. What we have in Africa is just the tip of the iceberg… We do not realize or have the full picture of the burden of monkeypox.”

A nurse examining a specimen sample from a child suspected of having monkeypox in the Democratic Republic of the Congo in July. (Source: Reuters).
What Makes This Outbreak Different?
Monkeypox is a viral disease related to the now-eradicated smallpox virus. According to the WHO, it can spread through close contact such as touching, kissing, or sexual intercourse, as well as through contaminated materials like bedding, clothing, and needles.
Initial symptoms often resemble the flu, including fever, chills, exhaustion, headache, and muscle aches, usually followed by a painful or itchy rash with raised lesions that crust over and heal within a few weeks.
Monkeypox is characterized by two genetic branches, I and II. Branch I is a broad group of viruses that have evolved over decades, showing significant genetic and clinical differences.
Branch II was responsible for a global outbreak declared a public health emergency from July 2022 to May 2023.
However, this new outbreak caused by branch I leads to more severe illness. The subgroup responsible for most of the current spread, branch Ib, is relatively new.
“Due to various factors, Ib has emerged as a new variant adapted to humans,” said Dr. Daniel Bausch, a senior advisor on global health security at FIND, a global nonprofit focused on health equity.
He explained that this virus typically spreads from animals to humans. But once it adapts, it can transmit between humans, leading to larger outbreaks.
Branch Ib is new and concerning, but the current situation is further complicated by overlapping outbreaks. “We are not just dealing with one outbreak of one branch; we are addressing multiple outbreaks of different branches in various countries with different modes of transmission and varying levels of risk,” said WHO Director-General Tedros on August 15.

A woman in Congo suffering from monkeypox with itchy lesions on her hands. (Source: AP).
How Dangerous Is the Disease?
According to the CDC, some outbreaks of branch I have resulted in a mortality rate of up to 10%, although recent outbreaks show lower fatality rates. The mortality rate for branch II is below 0.2%.
Certain groups, such as infants, individuals with severely weakened immune systems, and pregnant women, are more likely to experience severe infections. However, monkeypox surveillance remains inadequate, and there is still much to learn, Dr. Bausch noted.
“This is a virus that exists in the environment and is likely maintained in small mammals in Africa, and we really do not have appropriate diagnostic methods. It is not difficult to diagnose monkeypox infections when you have a laboratory next door, skilled lab personnel, and technology. But of course, most of these cases often occur in rural areas, so sampling and sending it to the lab is a challenging task,” he said.
According to him, our understanding of transmission potential and mortality risk may be skewed due to restrictions that tend to only detect the most severe cases. Regardless, the increasing spread will add to the burden on public health and the number of individuals affected.
“This is a disease that causes a lot of pain and suffering, a lot of fear, a lot of panic,” he remarked.

Currently, monkeypox is spreading to many countries in Africa, including those that have never reported the disease. (Source: AP).
Where Has Monkeypox Been Found?
For decades, monkeypox has primarily been found in Central and West Africa. Most cases of branch I originate from Central Africa and the Democratic Republic of the Congo, while most cases of branch II come from Nigeria.
In 2022, concerns increased as cases began to spread in Europe and North America. The widespread international spread is the main reason monkeypox was declared a global health emergency, but the geographic pattern of the current outbreak differs from that of the outbreak two years ago.
According to the Africa CDC, monkeypox is now spreading to many countries in Africa that were previously unaffected. While most cases remain concentrated in the Democratic Republic of the Congo, cases have also been reported in at least 13 countries across the continent.
On August 16, Sweden confirmed its first case of branch I monkeypox, marking the first time it has been detected outside of Africa.
Dr. Bausch cautioned against complacency until the outbreak is truly over, especially as international travel becomes more common. There are many reasons for concern, and early action is necessary.
He also mentioned the issues of fairness and human rights. The declaration of a global health emergency in 2022 set a precedent, and similarly, the transmission patterns in many African countries deserve attention and urgency just as much as the spread in high-income countries.

Vaccines are only part of the response to monkeypox. (Source: AP).
How to Prevent Spread?
Monkeypox vaccines are available, but they are not widely accessible in Africa. No cases of branch I have been detected in the U.S., but the CDC recommended last week that Americans who have been exposed or are at high risk for monkeypox should get vaccinated.
According to a detailed press release on August 16, the Gavi Vaccine Alliance has up to $500 million to spend on providing monkeypox vaccines to countries affected by the outbreak, including the Democratic Republic of the Congo and neighboring countries. Starting in 2026, Gavi will establish a global monkeypox vaccine stockpile, similar to existing stockpiles for cholera, Ebola, meningitis, and yellow fever vaccines.
But according to the WHO, vaccines are only part of the response; preventing the spread will also require enhanced surveillance, diagnostics, and research to fill “knowledge gaps.” The organization has signed off on the Emergency Use Listing process for both types of monkeypox vaccines and is developing a regional response plan requiring $15 million, of which $1.5 million is being disbursed from the WHO’s emergency reserve fund.
According to Tim Nguyen of the WHO Health Emergency Program, there are currently half a million doses of vaccines in reserve, and an additional 2.4 million doses could be produced by the end of this year.
Dr. Abdou Salam Gueye, Director of the WHO Regional Emergency Program for Africa, added that the Democratic Republic of the Congo and Nigeria will be the first countries to receive these vaccines.




















































