Jaw Osteitis in its early stages can be considered a mild bone joint disorder, but if not treated promptly, it can lead to more serious complications, including joint laxity.
Essential Information about Jaw Osteitis
- What is Jaw Osteitis?
- Signs to Identify Jaw Osteitis
- Causes of Jaw Osteitis
- At-Risk Groups for Jaw Osteitis
- Diagnosis and Treatment of Jaw Osteitis
- Treatment Methods for Jaw Osteitis
- Preventative Measures for Jaw Osteitis
- Frequently Asked Questions about Jaw Osteitis: Does Jaw Osteitis Affect Speaking Ability?
So how can we differentiate jaw osteitis from other jaw-related diseases? Let’s explore this article together.
What is Jaw Osteitis?
Jaw Osteitis is a condition that occurs when there is instability in the jaw joint and the surrounding muscles. It not only leads to chronic jaw pain but also causes muscle spasms, resulting in an imbalance in the skull and jawbone.
Jaw osteitis directly impacts daily activities, especially when speaking and chewing food.
Jaw pain restricts movements in the oral region.
Signs to Identify Jaw Osteitis
The signs of jaw osteitis are often mistaken for other oral issues due to similar symptoms. Therefore, clearly distinguishing the symptoms of this condition will help you seek timely treatment:
- Swollen gums, painful teeth
- Pain and swelling on one or both sides of the face. The pain may start mildly initially, allowing patients to manage it with painkillers, but it will progressively worsen as the condition advances
- Other symptoms: Pain in the ear area, neck stiffness, dizziness, hypertrophy of the chewing muscles, swollen lymph nodes, etc.
If you experience these symptoms and cannot identify the cause, please visit the nearest ENT or dental clinic for a thorough examination.
Causes of Jaw Osteitis
In addition to injuries or issues related to the jawbone and temporomandibular joint, which are the primary causes of jaw osteitis, several other factors can also contribute to this condition:
- Complications from tooth eruption: During the tooth eruption process, changes in the jawbone can create cavities that allow bacteria to invade. This is especially true when wisdom teeth erupt improperly, leading to gum coverage, food becoming trapped in the teeth, and bacteria potentially causing infections.
- Cavities: Untreated cavities can lead to pulpitis, periapical inflammation, soft tissue infections, or bone infections. The “decayed” environment in the cavity is ideal for bacterial growth and spread, resulting in jaw osteitis and soft tissue infections. Newly erupted milk teeth are less likely to cause soft tissue infections but can still lead to subperiosteal abscesses due to the short root length.
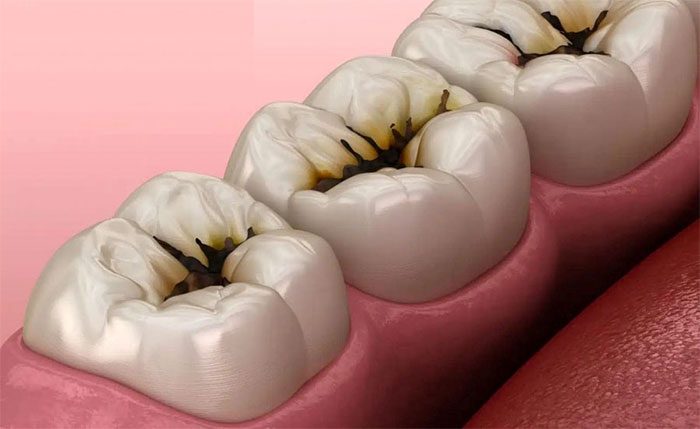
Cavities can also lead to jaw osteitis.
- Injury to the jaw area: Soft tissue injuries or trauma from broken teeth penetrating the tooth roots
- Tumors: Both benign and malignant tumors related to the jawbone can pose a risk of causing jaw osteitis
- Aging: The aging process accelerates with age, leading to wear on the bones and joints
- Other diseases that may lead to jaw osteitis: Measles, influenza, tuberculosis, syphilis, etc.
In addition to the above pathological causes, there are several habits that may seem insignificant but can lead to jaw osteitis in both the lower and upper jaws, such as:
- Teeth grinding: This action inadvertently creates significant pressure and stress on the temporomandibular joint, with prolonged and forceful grinding leading to jaw misalignment.
- Chelating food on one side: Frequently chewing food on one side of the jaw and consuming hard, difficult-to-chew foods can also place excessive pressure on the jawbone.
- Chronic stress: Unstable moods and psychological pressure can lead to uncontrolled jaw muscle contractions and create a habit of grinding teeth during sleep.
Many may perceive these as minor bad habits that are not serious, but they can significantly impact the development of the jawbone. Strive to minimize these habits and maintain a healthy lifestyle to protect your oral health.

Frequent teeth grinding creates pressure on the jawbone.
At-Risk Groups for Jaw Osteitis
Jaw osteitis is a condition related to teeth and jaw, so it can occur in all demographics, from adults to children. Although women during puberty and perimenopausal periods are at a higher risk, this does not mean that men should be complacent, as anyone can be affected by this condition.
What Complications Can Arise if Jaw Osteitis is Left Untreated?
Although it is not life-threatening or severely dangerous, jaw osteitis can lead to several other complications if not treated promptly:
- Joint laxity: This condition increases the risk of joint dislocation and joint locking.
- Spread to the submandibular region: Swelling in the submandibular area can extend to other areas such as the neck and chest. This may cause the mouth to remain open, with the tongue elevated, making it difficult to breathe and swallow.
- Jawbone deformity: Areas of inflamed muscle and bone can be severely affected if not treated promptly, leading to structural breakdown and deformity.
Diagnosis and Treatment of Jaw Osteitis
Diagnosis of jaw osteitis
Clinical Diagnosis
Here are some clinical manifestations of jaw osteitis that you may observe:
- Swollen and red cheeks
- Cavities, with necrotic pulp causing pain
- Skin in the surrounding area may be discolored, and pus may ooze from the swollen region
- Possible signs of mild or high fever
Paraclinical Diagnosis
In addition to clinical diagnosis, doctors may perform additional tests to further assess the condition of the bones and joints:
- X-ray: To identify the cause of jaw inflammation
- Blood tests before surgery: To check for elevated white blood cell counts
Treatment Methods for Jaw Osteitis
Medication
Like other medical conditions, medication is an effective and common method for treating jaw osteitis. Not only does it help relieve pain and swelling in the jaw area, but it also has anti-inflammatory properties and prevents complications from the disease. Here are some medications that doctors may prescribe:
- Pain relievers, such as paracetamol, mobic, diclofenac, etc.
- Anti-inflammatory drugs, such as corticosteroids
- Muscle relaxants for short-term use
- Injectable medications to relieve pain from temporomandibular disorders
The above are just a few reference medications. For accurate and suitable treatment, please consult directly with a qualified doctor or pharmacist for the most appropriate treatment methods.

It is advisable to take medications as prescribed by your doctor.
Non-Medication Approaches
For more severe cases of jaw osteitis, certain methods and procedures may be required to address the condition:
- Surgery: This is considered a last resort when other treatment methods do not achieve the desired results. Surgery will help to thoroughly repair or replace the damaged joint.
- Dental treatment: Adjusting the bite, tooth extraction, dental implants, or fillings if necessary. Orthodontic treatment may cause some discomfort but helps improve the condition and function of the jawbone.
- Arthrocentesis: This procedure aims to remove small fragments causing inflammation in the joint, helping to reduce damage to the bone.
These surgical procedures require high expertise, so patients should seek reputable and professional locations to ensure safety during treatment.
Preventive Measures for Jaw Osteitis
Jaw osteitis can also be prevented and improved by practicing the following healthy habits:
- Prioritize soft, easy-to-chew foods.
- Avoid chewing on one side of the jaw.
- Limit harmful habits such as teeth grinding and jaw clenching.
- Massage the area under the chin for about 15 minutes each day to relax the muscles and improve blood circulation.
- Choose reputable dental clinics and hospitals for treatment.
- Balance sleep and rest time to maintain a relaxed state of mind, reducing pressure and stress.
- Never self-prescribe medication or use folk remedies, and do not use someone else’s prescription as individual conditions vary.
Common Questions About Jaw Osteitis
Does jaw osteitis affect speaking ability?
Jaw osteitis can cause pain when opening the mouth and may affect speaking and swallowing abilities.
What should I do if medication hasn’t alleviated the condition?
Visit the nearest dental clinic for a check-up and to receive the most accurate treatment solution. Do not let the condition worsen, as it could lead to dangerous complications.
How much does the treatment for jaw osteitis cost?
The cost depends on individual cases, the severity of the infection, and the patient’s body condition, leading to different treatment processes. Although jaw osteitis is not overly dangerous, it can directly impact your quality of life and daily activities. If you are uncertain about your condition, visit the nearest hospital for proper diagnosis and treatment.




















































