Bronchiectasis (BE) is a common respiratory disease, especially during the cold season. If not detected and treated promptly, it can lead to many dangerous complications. This condition is characterized by an irreversible dilation of the bronchial tubes. The dilation may occur in the larger bronchi while the smaller ones remain normal, or vice versa.
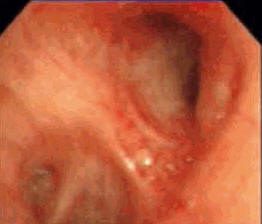 |
Left upper lobe bronchus |
Patients with BE typically exhibit characteristic symptoms such as chronic cough, sputum production, and hemoptysis (coughing up blood). The cough is persistent, with significant purulent sputum production daily, and the breath often has a foul odor. The sputum consists of three layers: the top is frothy, the middle is purulent, and the bottom is mucous.
Hemoptysis may occur (ranging from mild to severe). In cases of BE in children, instances of hemoptysis are less common. Chest pain may be an early sign of bronchial infection in the BE-affected area. Patients may also experience recurrent pneumonia in the BE region.
Moreover, one-third of patients with this condition may exhibit clubbing fingers. Patients often experience weight loss, anemia, and fatigue, with 80% showing accompanying upper respiratory symptoms such as rhinitis and purulent sinusitis. If BE is widespread in both lungs, patients may experience cyanosis and difficulty breathing. In the affected lung areas, recurrent pneumonia may occur frequently, especially during the cold season.
Upon auscultation, localized wheezing is often heard in areas affected by BE, typically at the bases of the lungs. If there is concurrent bronchial obstruction, diffuse wheezing may be heard in both lungs or a high-pitched wheeze may be present. If localized crackles or rales are frequently heard at the lung bases while chest X-rays appear normal, BE should be suspected.
Post-infectious BE is commonly found in the upper lobes (due to pulmonary tuberculosis or lung abscess). Common complications of BE include pneumonia, lung abscess, and chronic cor pulmonale…
Some less common symptoms include:
– Vasculitis with skin petechiae.
– BE may accompany several conditions such as sinusitis, rheumatoid arthritis, chronic colitis, infertility (infertility is a symptom of cystic fibrosis, primary ciliary dyskinesia), yellow nail syndrome, connective tissue diseases (systemic lupus erythematosus), vasculitis with skin hemorrhages, and increased circulating immune complexes, etc.
What causes bronchiectasis?
Congenital bronchial structural defects: Diffuse BE along with sinusitis and organ malposition (heart displaced to the right) due to dysfunction of bronchial cilia.
Defects or absence of cartilage in the bronchi lead to bronchial dilation on inhalation and collapse on exhalation. When the bronchi become hypertrophied due to structural connective tissue defects, it is accompanied by BE.
Due to necrotizing inflammation in the bronchial wall: BE can occur after lung infections such as tuberculosis, bacterial pneumonia, viral infections, measles, whooping cough, or due to aspiration of gastric contents or blood, inhalation of toxic smoke (ammonia gas), or recurrent bronchial infections.
Due to cystic fibrosis: This accounts for 50% of BE cases and is the most common cause in Europe and North America.
Due to obstruction of the large bronchi: bronchial lymph node tuberculosis, or foreign bodies lodged in the bronchi in children, bronchial tumors, or fibrous scarring causing bronchial stenosis after trauma to the large bronchi. Below the site of bronchial stenosis, intrabronchial pressure increases, leading to secretions accumulating and causing chronic localized infection, which then develops into BE.
Due to fibrotic or granulomatous lesions pulling on the bronchial wall: fibrotic pulmonary tuberculosis, cavitary fibrotic tuberculosis, chronic lung abscess, and fibrotic interstitial pneumonia. BE in post-primary tuberculosis can develop through two mechanisms:
– Most commonly due to destruction and fibrosis of lung parenchyma leading to retraction and irreversible BE.
– Bronchial stenosis due to scarring after localized bronchial tuberculosis. Since most cases of post-primary tuberculosis involve lesions in the apical segments and posterior segments of the upper lobes, BE is often found in these areas, which are well-drained bronchially, hence the symptoms are often mild. Hemoptysis is commonly seen in this form of BE.
Disruption of mucociliary clearance: BE may develop in cases of secondary ciliary motility disorders associated with bronchial asthma. In these cases, bacteria may proliferate in the lower respiratory tract.
Disruption of pulmonary protection mechanisms:
Immunodeficiency, either congenital or acquired, such as hypogammaglobulinemia, selective IgA, IgM, or IgG deficiency.
Acquired (secondary) immunodeficiency: due to cytotoxic drug use, HIV/AIDS infection, bone marrow disease, chronic leukemia.
Idiopathic bronchiectasis: It is believed that idiopathic BE may be due to overlooked pulmonary clearance disorders, commonly seen in adults in the lower lobes.
Treatment: It is essential to eliminate all bronchial irritants: tobacco and shisha; identify and treat any sources of oral, ear, nose, and throat infections; administer influenza and pneumococcal vaccines.
Respiratory rehabilitation is crucial: this should be done regularly with breathing exercises, controlled coughing, and chest percussion to facilitate sputum drainage, lying in various positions to enhance drainage according to the affected bronchial regions multiple times a day; inhaled bronchodilators stimulating beta-2 receptors (such as salbutamol, terbutaline, etc.). In cases of fever, excessive sputum production, purulent sputum, or complications from parenchymal or pleural infections, antibiotics should be used as prescribed by a physician.
Bronchoscopy may be performed to diagnose the bleeding site, clear obstructive secretions from the bronchi, and release lesions causing bronchial obstruction. Surgical intervention is indicated for localized BE in one lung when there is significant purulence or severe hemoptysis, especially if medical treatment fails. Worldwide, lung transplantation is beginning to be applied in the treatment of BE.
Prevention: It is important to maintain good hygiene for the respiratory system. If children are infected with bronchial infections, thorough treatment is necessary. Adults should also maintain oral and nasal hygiene. If suffering from rhinitis or sinusitis, complete treatment is essential to prevent complications leading to BE.



















































