Restless Leg Syndrome (RLS) particularly worsens with seasonal changes – here’s what you need to know.
Key Facts About Restless Leg Syndrome
- 1. What is Restless Leg Syndrome?
- 2. Symptoms of Restless Leg Syndrome
- 3. Causes of Restless Leg Syndrome
- 4. Risk Factors for Restless Leg Syndrome
- 5. Diagnosing Restless Leg Syndrome
- 6. Home Remedies for Restless Leg Syndrome
- 7. Medications for Restless Leg Syndrome
- 8. Diet for Individuals with Restless Leg Syndrome
1. What is Restless Leg Syndrome?
Restless Leg Syndrome (RLS), also known as Willis-Ekbom Disease, is a common movement disorder and sleep disorder characterized by an overwhelming urge to move the legs, often accompanied by uncomfortable sensations. This urge is usually strongest when the individual is resting or trying to sleep.
Overall, RLS is categorized as a sensory neurological disorder with symptoms originating from the brain.
According to Healthline, about 80% of individuals with RLS experience a related condition known as Periodic Limb Movement Disorder (PLMD), which involves involuntary jerking or twitching of the limbs every 1 to 40 seconds during sleep, often disrupting nighttime rest and causing daytime sleepiness.
Can Restless Leg Syndrome be cured? The answer is no. RLS is a lifelong condition without a definitive cure; however, symptom management strategies can help individuals feel more comfortable and reduce the impact on sleep quality.

Restless Leg Syndrome (RLS), also known as Willis-Ekbom Disease, is a common movement and sleep disorder. (Image: Internet).
2. Symptoms of Restless Leg Syndrome
The most prominent symptom of RLS is an overwhelming urge to move the legs, particularly when sitting still or lying down in bed trying to sleep. Individuals may also experience unusual sensations such as tingling, crawling, or a desire to stretch the calves to alleviate these feelings.
If you experience mild RLS, these symptoms may not occur every night, and many confuse the restlessness with stress or anxiety. Symptoms may come and go.
For those with more severe RLS, sitting still to watch a movie or during long flights can be quite challenging.
Difficulty sleeping and insomnia due to more pronounced symptoms at night can lead to increased daytime sleepiness, fatigue, and negative impacts on both physical and mental health.
Symptoms of RLS can affect both sides of the body, though some may only experience them on one side. The most commonly affected body parts include the arms and legs. Symptoms may also worsen with age.
3. Causes of Restless Leg Syndrome
According to Healthline, about 40% of individuals with RLS have a family history (genetic factors), and symptoms often begin before the age of 40.
Low brain iron levels may also be associated with RLS (blood tests may still show normal iron levels).

There are various causes of Restless Leg Syndrome. (Image: Internet).
Disruptions in dopamine transmission in the brain are also linked to RLS, such as in Parkinson’s disease – this partly explains why many individuals with Parkinson’s experience RLS. Dopamine is involved in controlling muscle movement and may be the cause of the involuntary leg movements associated with RLS.
In addition to the above causes, some stimulants such as caffeine or alcohol can trigger or exacerbate RLS symptoms.
If you are taking medications for allergies, nausea, depression, or psychiatric disorders, you may also experience restless legs.
On the other hand, RLS may also be a “branch” of an existing health issue, such as neuropathy, diabetes, or kidney disease. In such cases, managing and treating the primary condition may resolve RLS symptoms.
4. Risk Factors for Restless Leg Syndrome
There are certain conditions that may increase your risk of developing RLS compared to others. According to Healthline, factors to consider include:
- Gender: Women are twice as likely to develop RLS compared to men.
- Age: Although RLS can occur at any age, it tends to be more common and severe after middle age.
- Family History: Genetic factors are considered one of the risks for developing RLS if there is a family history of the condition.
- Pregnancy: Some women experience RLS during pregnancy, particularly in the third trimester, but symptoms typically decrease and disappear within a few weeks after childbirth.
- Chronic Conditions: Chronic conditions such as peripheral neuropathy, diabetes, and kidney disease may lead to RLS. Treating these conditions can help alleviate RLS symptoms.
- Medications: Antinausea medications, antipsychotics, antidepressants, and antihistamines may cause or worsen RLS symptoms.
If you have RLS and chronic insomnia, you may also be at higher risk for conditions such as heart disease, stroke, diabetes, kidney disease, depression, and increased mortality.
5. Diagnosing Restless Leg Syndrome
There is no specific test to confirm or exclude RLS. Most diagnoses are based on the description of the symptoms you experience, including:
- 1. An overwhelming urge to move accompanied by feelings of restlessness, discomfort, and unease.
- 2. Symptoms worsen at night and improve or disappear in the early morning.
- 3. Symptoms are triggered when you try to relax, rest, or sleep.
- 4. Symptoms diminish when you move.
Even if these conditions are met, you should still seek a health examination to rule out other neurological reasons that may cause similar symptoms. Don’t forget to discuss with your doctor the medications you are taking, your sleep conditions, medical history, family history, etc. Blood tests may also be prescribed to evaluate and check for iron levels or other unusual nutritional deficiencies.
6. Home Remedies for Restless Leg Syndrome
While home remedies cannot completely eliminate symptoms, they can help you feel more comfortable. You may try one or more coping strategies to find what works best for your condition:
- Reduce or eliminate caffeine, alcohol, and tobacco intake.
- Try to maintain a regular sleep schedule, going to bed and waking up at the same time each day, and ensure good sleep hygiene, including a cool room temperature, a dark environment, and clean bedding.
- Engage in daily exercise, such as walking, swimming, yoga, or meditation, which can also support sleep.
- Massage or stretch your calf muscles in the evening.
- Take a warm bath before bed.
- Use a hot or cold compress when symptoms occur.
- For pregnant women, consider the risk of iron deficiency through blood tests. At home, avoid sitting still for long periods, especially in the evening; engage in light exercise regularly; avoid antihistamines, caffeine, tobacco, and alcohol; some RLS medications are not safe during pregnancy. Consult your doctor for appropriate advice.
- If you need to travel for extended periods, try to plan your travel during the day.
- Consult with a nutritionist if RLS is due to nutrient deficiencies to receive dietary supplementation advice tailored to your condition. However, do not self-supplement with supplements without a doctor’s recommendation.
Sleep and exercise recommendations for individuals with Restless Leg Syndrome:
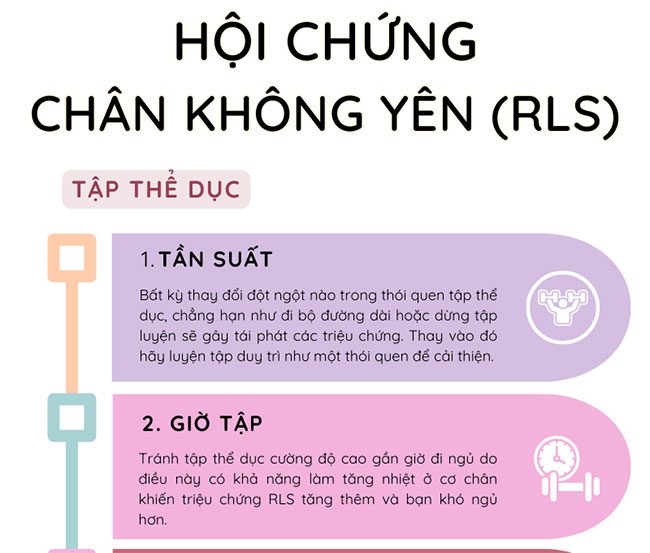
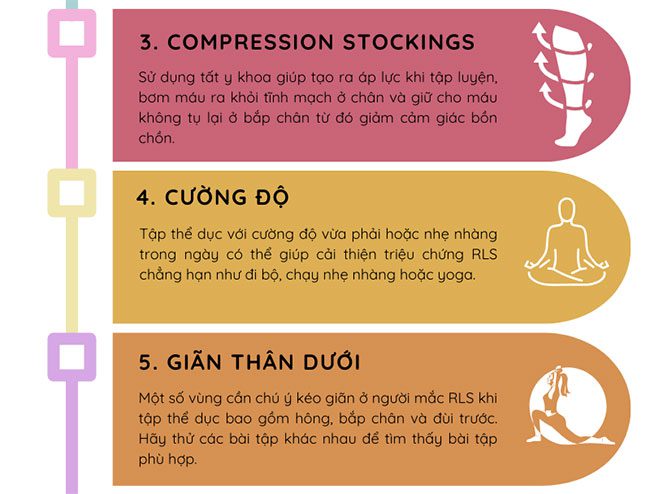

Image: Kim Phung SKHN
7. Medications for Restless Legs Syndrome
Medications can help alleviate and control the symptoms of Restless Legs Syndrome (RLS). Here are some options you may consider:
- Dopamine agonists including pramipexole, ropinirole, and rotigotine. Possible side effects include transient dizziness and nausea. Over time, these medications may become less effective and may cause daytime sleepiness or exacerbate RLS symptoms.
- Sleep aids and muscle relaxants (benzodiazepines) can help you relax and sleep better but may cause daytime drowsiness as a side effect.
- Opioid pain relievers and anti-anxiety medications are powerful and may be addictive. Side effects can include dizziness and nausea, and these medications are not recommended for individuals with sleep apnea.
- Anticonvulsants can help alleviate sensory disturbances. Side effects may include dizziness and fatigue.
In general, you should not take any medication without a doctor’s prescription, and you may need to try more than one type of medication to find the right one for you.

Many cases will be prescribed medication to alleviate symptoms. (Image: Internet).
8. Diet for Individuals with Restless Legs Syndrome
There are no specific dietary guidelines for individuals with Restless Legs Syndrome. However, it is important to review your diet to ensure you are consuming a balanced intake of essential vitamins and minerals. Try to reduce processed foods high in calories but low in nutritional value (empty calories).
If you have RLS due to a deficiency in a specific vitamin or mineral, some dietary changes may help alleviate and treat the condition. If you are iron deficient, consider incorporating iron-rich foods such as dark leafy greens, red meat, poultry, seafood, cereals, and bread. Don’t forget to pair these with vitamin C to help your body absorb iron more effectively.
Foods rich in vitamin C include citrus fruits, broccoli, tomatoes, peppers, and dark leafy greens.
Check if caffeine or alcohol aggravates your Restless Legs Syndrome symptoms and consider reducing or eliminating these stimulants—especially for those affected by sleep disturbances.
Above are some insights into Restless Legs Syndrome and related treatment considerations for alleviating symptoms of restlessness and discomfort. If you have any questions, you should consult a doctor for appropriate advice.


















































