This virus is known as herpes simplex virus type 1. It differs from most other viruses in that it can invade the nervous system. Most people may not exhibit any symptoms after infection, but some unfortunate individuals can suffer from blindness or life-threatening encephalitis when infected with this type of virus.
Therefore, the academic community has paid close attention to the infection mechanisms of this particular virus. Scientists have known that after the virus enters a cell, it relies on certain motor proteins to transport it to the nucleus, where it can replicate; however, they have yet to determine how this virus controls the molecular motors.
Now, a research team has discovered a strange phenomenon: the virus will take a motor protein from the initially infected cell and activate it. When the next wave of infection is about to occur, scientists have uncovered its secret of movement. They published their research findings in the journal Nature.
If a human cell is likened to a city, then within this city, there are many different molecules (proteins, nucleic acids, etc.) that must move between various blocks, making roads and transportation essential. There is a railway called microtubules in the cellular city, which serves as a “road” for many substances; there are several motor proteins that run along this road, acting as “vehicles” for those substances.
When the virus invades cells, it too must use this transport system to travel from an indeterminate corner to the city center: the nucleus. Only by penetrating the cell nucleus can the virus mix its genetic material with the cell’s original DNA, allowing the cell to produce the materials necessary for the virus to replicate. As a result, the cell becomes a virus production factory, contributing to subsequent infection processes.
However, if the virus infects a nerve cell, it may not be as easy as infecting other cells. Nerve cells have very long tails known as “axons.” If the virus invades from the tip, it must traverse the long microtubules to reach the cell body of the neuron before it has the chance to “transmit to the nucleus.”
Nerve cells have very long tails.
Thus, not every type of virus has the ability to attack the nervous system. However, herpes simplex virus type 1, as well as rabies virus or pseudorabies virus, can do so, and these viruses are referred to as “neurotropic viruses.” Scientists want to know if such viruses possess certain common capabilities when they utilize motor proteins for self-transport.
As mentioned earlier, there is a type of pathway in the cell called “microtubules.” There are two types of motor proteins that run along this pathway, one known as dynein and the other as kinesin. The virus will capture them and can move along the pathways of these protein types. Among the two types of motor proteins, kinesin is particularly significant for neurotropic viruses.
Scientists first infected human retinal pigment epithelial (RPE) cells with herpes simplex virus type 1 (HSV-1). If you wonder why epithelial cells were used, it’s because compared to nerve cells, epithelial cells are in direct contact with the external environment and often suffer from viral attacks, making them the most realistic choice.
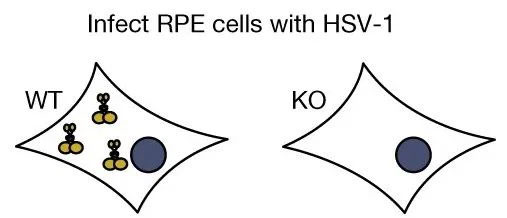
Infected cells with HSV-1 virus, normal epithelial cells on the left and epithelial cells lacking kinesin on the right.
The result of this initial infection was: When normal epithelial cells were infected by HSV-1, most of the virus capsid remained on the nuclear membrane, indicating that those viruses had successfully entered the nucleus; however, when the cells lacked kinesin, the virus capsid would accumulate in the cytoplasm in large quantities, meaning fewer viruses entered the nucleus.
Scientists believe that during the first infection, kinesin in the cells may help the virus enter the nucleus.
Next, it was time for a second infection. This time, the research team would grow HSV-1 in epithelial cells and then use these viruses to infect primary sensory neurons. Among them, a portion of the virus was cultured in normal epithelial cells (with kinesin), and another portion of the virus was cultured in kinesin-deficient epithelial cells. However, the neurons they aimed to attack all had their own kinesin.
Given that there are kinesins in the nerve cells, when the two groups of viruses attack the nerve cells, will they be able to enter the nucleus favorably?
However, the results of the second infection were not as expected. The virus cultured in normal epithelial cells was used to infect the nerve cells. Most of the capsids were on the nuclear membrane, indicating that a large number of viruses had entered the nucleus; and the virus gathered in kinesin-deficient epithelial cells could reach the nerve cells.
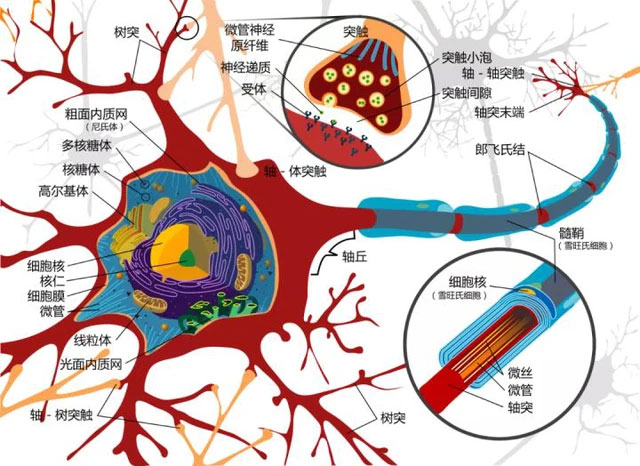
Diagram of neuron structure, the yellow sphere is the nucleus.
In other words, even with kinesin present in the environment during the second infection, it could not compensate for the lack of kinesin during the first infection. With this in mind, scientists hypothesize that the virus may have extracted some kinesins from the epithelial cells during the first infection, which would be used in the subsequent infection.
The researchers relied on these experiments to demonstrate that HSV-1 had indeed taken kinesin from the epithelial cells outside the cell. During the subsequent infection of nerve cells, the virus actually utilized them.
Specifically, the scientists created special substitutes for the common kinesins in epithelial cells and then applied a type of drug to the nerve cells that could immobilize the virus carrying these special kinesins on their trajectories (microtubules). As a result, the virus cultured in these epithelial cells showed a reduced ability to infect nerve cells, which sufficiently indicated that the virus depended on kinesin stolen from epithelial cells and found it difficult to replace kinesin in nerve cells.
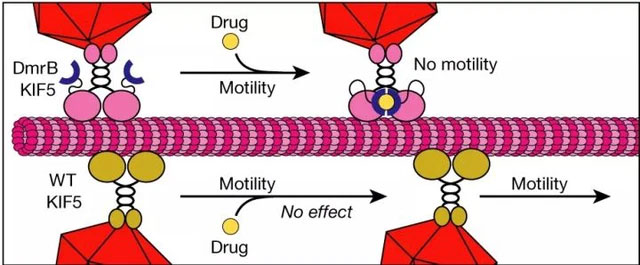
Scientists explain that after HSV-1 acquires kinesin from epithelial cells, it will assimilate it into a part of itself, giving it a new utility – originally a type of protein that transports cargo for cells, but after being “hijacked” by the virus, it only serves to facilitate the virus’s movement.
The researchers still do not understand why there are kinesins in nerve cells, but the virus must “hijack” the proteins from epithelial cells for use. However, the ability to uncover how herpes simplex virus type 1 utilizes motor proteins has greatly excited scientists.
The journey from the end of the neuron to the cell body takes about 8 hours, and while traversing the long axon of the neuron, the virus primarily relies on dynein. In contrast, many common viruses, when ready to move to the next cell, carry little more than their own proteins.
The reason scientists are particularly interested in herpes simplex virus type 1 is that once they invade the nervous system, it is almost impossible to eliminate them.

Cold sores, most patients infected with HSV-1 may not experience symptoms.
Although after most people are infected, the virus remains dormant or latent and shows no clear symptoms; some individuals may experience recurrent infections after the peripheral nervous system is invaded; and a few may suffer attacks on the central nervous system (brain or spinal cord), leading to damage and even life-threatening conditions.


















































