Early Childhood Caries (ECC) is highly prevalent, affecting 30-50% of children in developing countries and up to 70% in developed nations. Children who experience tooth decay at a young age are at greater risk of dental issues as they grow older, making early prevention crucial to avoid significant oral health problems later in life.
Pathogenesis
 |
|
(Image: qualitydentistry) |
Caries formation is influenced by organic acids produced from the fermentation of carbohydrates in food, which bacteria use to lower the pH in dental plaque, resulting in mineral loss. Initial carious lesions appear as white spots on the enamel, and cavities develop as the demineralization progresses.
The group of bacteria known as Streptococcus mutans is associated with caries development. These bacteria adhere to the enamel, producing acids and thriving in low pH environments. Once the enamel is breached, other bacteria (such as Lactobacillus) proliferate, creating an acidic environment that accelerates demineralization. The extent of acid-induced demineralization heavily depends on the frequency and type of carbohydrates consumed.
Symptoms and Signs
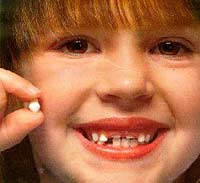
Tooth decay in primary teeth often begins in the pits and fissures. Small lesions can be difficult to detect with the naked eye; however, larger lesions typically manifest as cavities on the chewing surfaces. The second most common location for cavities is on the proximal surfaces (the contact points between teeth), with many cases only detectable via dental X-rays. Lesions on smooth surfaces (the outer and inner surfaces) are usually seen in children with severe decay.
Severe early childhood caries is recognized as Early Childhood Caries (ECC), baby bottle tooth decay, or nursing bottle caries, often inaccurately associated with bottle feeding. While the interplay between bacterial infection and sugar consumption is crucial in children, other factors such as enamel hypoplasia due to prenatal malnutrition or prematurity also play significant roles in the development of caries.
ECC is quite common, with cases appearing as early as 12 months, often months before a child sees a dentist. Risk factors for ECC include frequent sugar consumption (from sweet drinks or snacks), immigrant status, having family members (parents or siblings) with dental caries, and dental anomalies.
Complications
If untreated, tooth decay can lead to complete destruction of the affected tooth and possible pulp damage, resulting in pulpitis and pain. Pulpitis may progress to necrosis, allowing bacteria to invade the surrounding bone and cause dental abscesses. Infections in primary teeth can affect the eruption of permanent teeth. In some cases, primary tooth infections may lead to sepsis or facial infections.
Treatment
The age of the child at the time of decay is significant for dental treatment. Children under 3 years of age often cannot cooperate during dental procedures and typically require support such as restraint, anesthesia, or sedation for fillings. After age 4, children can generally respond better to dental treatment and local anesthesia.
Dental treatments may include silver amalgam, composite fillings, or crowns to preserve decayed teeth. If the decay extends to the pulp, partial or complete pulpectomy may be necessary. If a tooth must be extracted, preserving the space is essential to prevent the shifting of remaining teeth, which can lead to misalignment of permanent teeth later.
Localized infections in the bone can be managed through localized treatments (tooth extraction, complete pulpectomy). Oral antibiotics are indicated for cases of tooth infections with cellulitis, facial swelling, or when local anesthesia cannot be administered due to inflammation. Penicillin is the preferred antibiotic unless there is a history of allergy, in which case clindamycin or erythromycin may be used. Oral analgesics like ibuprofen are generally effective for pain management. In severe cases of widespread infection threatening the child’s life, injectable antibiotics may be required.
Prevention
The most effective means of preventing caries is to provide optimal fluoride levels in drinking water at a concentration of 1 ppm. Children living in areas with fluoride-deficient water are at higher risk for caries and may need fluoride supplements. To avoid fluoride overdose, physicians should not prescribe more than 120 mg of fluoride. Acute manifestations of fluoride overdose (above 5 mg/kg) require emergency intervention. Topical fluoride applications (administered by the dentist or caregiver) are beneficial for at-risk children.
Oral Hygiene
Daily brushing, particularly with fluoride toothpaste, helps prevent tooth decay. Most children under age 8 do not brush effectively. Therefore, parents play a crucial role in ensuring their children maintain good oral hygiene and develop positive habits.
Diet
Reducing the frequency of sugary food and drink consumption is an effective preventive measure against tooth decay. Children should not be given sweet beverages or foods at night; for those at high risk of caries, it is advisable to avoid snacks between meals.
Pit and Fissure Sealants
Resin-based pit and fissure sealants have been shown to effectively prevent tooth decay in primary and permanent molars. The best results are achieved when sealants are placed immediately after teeth erupt (typically at ages 1-2) and in cases of deep grooves or fissures in molars.
Dr. NGÔ LÊ THU THẢO


















































