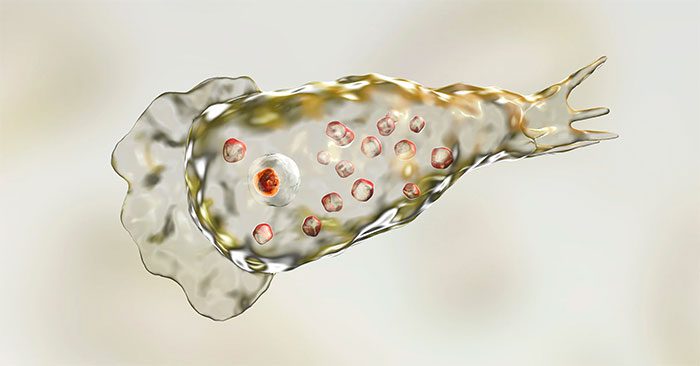
The brain-eating amoeba, scientifically known as Naegleria fowleri, is a type of parasite. This rare parasite is often lethal to those who swim or participate in water sports in freshwater lakes, rivers, and hot springs.
Essential Facts About Naegleria fowleri (Brain-Eating Amoeba)
Amoebas known as Naegleria fowleri ascend through the nose to the brain, causing severe damage. Most infected individuals die within a week of infection.
Millions of people are exposed to the Naegleria amoeba each year, but only a few develop the disease. Scientists have not yet explained why some people become infected while others do not.
Causes of Brain-Eating Amoeba Disease
The brain-eating amoeba disease is caused by infection with the Naegleria fowleri amoeba, commonly found in freshwater lakes worldwide. The disease is more prevalent during summer, and the amoeba can also be found in soil.
Amoebas enter the body through the nose when it comes into contact with contaminated water or dirt and travel to the brain via the olfactory nerve.
Not everyone who contacts the amoeba becomes ill; only a small percentage of the millions who encounter Naegleria fowleri develop the disease.
Symptoms of Brain-Eating Amoeba Disease
When infected with Naegleria, individuals develop a condition known as Primary Amebic Meningoencephalitis, characterized by inflammation of the brain and destruction of brain tissue. Symptoms typically begin 2 to 15 days after infection and may include:
- Altered sense of smell or taste
- Fever
- Sudden severe headache
- Stiff neck
- Light sensitivity
- Nausea and vomiting
- Loss of balance
- Confusion
- Sleepiness
- Seizures
- Hallucinations
These symptoms progress rapidly and can lead to death within about a week.

Transmission Pathways of Brain-Eating Amoeba Disease
The amoeba does not spread from person to person or from an infected individual to water. Properly cleaned and disinfected swimming pools do not harbor Naegleria fowleri.
At-Risk Groups for Brain-Eating Amoeba Disease
In the United States, millions of people are exposed to the Naegleria amoeba each year, but very few become ill. From 2007 to 2017, only 40 cases of infection were reported. Some factors that may increase the risk of Naegleria infection include:
Swimming in warm freshwater lakes or pools. Most infected individuals had swum in freshwater lakes within the past two weeks.
The amoeba thrives in warm or hot water, with an ideal temperature around 35 degrees Celsius. This parasite proliferates during summer as water temperatures rise.
In Vietnam, many believe that bathing in warm or hot water is beneficial for health; however, these conditions are also conducive for the brain-eating amoeba to thrive due to the typically warm water in downstream areas.
Children and teenagers are the most susceptible age groups, possibly because they spend more time in the water and are more active, allowing the amoeba time to travel from the nose to the brain.
Prevention of Brain-Eating Amoeba Disease
The Centers for Disease Control and Prevention (CDC) suggests measures to reduce the risk of Naegleria infection:
- Avoid swimming in or jumping into warm freshwater lakes.
- Pinch the nose or use nose clips when jumping or diving into warm water.
- Avoid stirring up sediment in shallow, warm water while swimming.
- Diagnostic Measures for Brain-Eating Amoeba Disease
CT scans or MRIs may reveal swelling and bleeding in the brain:
- CT Scan: This technique combines X-ray images from multiple angles to create detailed cross-sectional images of the brain to identify damaged areas.
- MRI: MRI machines use radio waves and strong magnetic fields to produce extremely detailed images of soft tissues, such as the brain.
- Lumbar Puncture: Naegleria amoeba can be viewed under a microscope using lumbar puncture techniques. Doctors will extract cerebrospinal fluid from the L2-S2 vertebrae while measuring cerebrospinal fluid pressure to assess whether the patient has increased intracranial pressure.
Treatment Options for Brain-Eating Amoeba Disease
Very few infected individuals survive Naegleria infections, even with treatment. Early detection, diagnosis, and treatment are critical for patient survival.
The primary treatment for Naegleria infection is antifungal medication, such as amphotericin B, administered intravenously or injected around the patient’s spinal cord to kill the amoeba.
A drug currently being tested called miltefosine is used for emergency treatment of Naegleria infections. When used alongside other medications and in conjunction with controlling cerebral edema, it may increase the chances of survival for patients.