When bilirubin, a byproduct of red blood cell breakdown, accumulates in the blood and deposits in the skin and mucous membranes, it causes jaundice.
 |
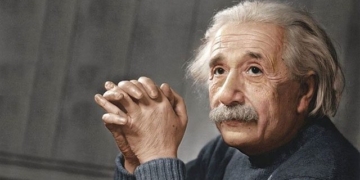
| Treating jaundice in children with “light therapy” in the neonatal emergency room at Tuyen Quang General Hospital. (Photo: Youth) |
Jaundice can arise from various causes. Children of any age can develop jaundice, particularly newborns.
Here are some common causes:
Physiological Jaundice: Typically appears between the second and fourth day after birth and resolves within 10 days. If jaundice persists for more than three weeks, it is usually not physiological jaundice, and other pathological causes should be investigated. Physiological jaundice does not require treatment.
Jaundice Due to Infection: The most common type in newborns is umbilical infection and skin infection. Jaundice may appear early or late. Affected infants often have fever (sometimes low body temperature), yellow urine, weak crying, poor feeding, vomiting, and diarrhea. In this case, infants should continue breastfeeding as much as possible. They need to be treated with specific antibiotics and symptomatic care at healthcare facilities as directed by a physician. The most effective preventive measure is to practice good aseptic techniques during delivery and care for the umbilical cord to prevent infection.
Jaundice Due to Syphilis: This occurs when a child contracts syphilis from the mother. Symptoms typically appear after birth. Jaundice is usually mild but prolonged and is accompanied by hepatomegaly and splenomegaly. The child may show signs of congenital syphilis. An important diagnostic factor is the medical history of the parents. If there are any suspicious signs, the child should be taken to a healthcare facility for diagnosis and treatment. If detected early and treated promptly, the condition can progress positively.
Jaundice Due to Viruses: Mainly caused by viruses that lead to hepatitis transmitted from mother to fetus through the placenta. Common symptoms include prolonged jaundice, yellow urine, occasionally pale stools, and hepatomegaly. Children need to be taken to healthcare facilities for examination, treatment, and counseling similar to other cases of viral hepatitis.
Hemolytic Jaundice Due to Rh Incompatibility: This occurs when the mother is Rh negative, the father is Rh positive, and the child is born Rh positive. In this case, during pregnancy, some Rh positive fetal red blood cells pass through the placenta into the Rh negative mother’s bloodstream. The mother’s body reacts by producing antibodies against Rh positive cells. These antibodies cross the placenta into the fetus’s body and cause hemolysis. The frequency of this condition depends on the proportion of women with Rh negative blood.
In our country, very few women are Rh negative, so this condition is rare. It is more commonly seen in multiparous women than in primiparous women. Jaundice appears in the early days after birth and lasts for several weeks, along with symptoms of anemia, bleeding, hepatomegaly, and splenomegaly.
In cases of kernicterus, affected infants display neurological symptoms such as jaw stiffness, muscle rigidity, and cyanosis. These cases are often severe and can lead to death. Children need to be treated in specialized pediatric centers with “exchange transfusions” and intensive care. When Rh incompatibility is detected, the mother requires monitoring and counseling from specialized healthcare providers.
Hemolytic Jaundice Due to ABO Incompatibility: This usually occurs when the mother has blood type O and the child has type A or sometimes type B. The condition is more common if the cause is Rh factor incompatibility but rarely leads to kernicterus. The condition tends to progress well with treatment.
Jaundice Due to Congenital Biliary Atresia: This condition results from varying degrees of narrowing of the bile ducts. Moderate jaundice typically appears in the second week after birth. The jaundice is dark in color and continuous, associated with pale stools, dark urine, hepatomegaly, and splenomegaly. Patients need early diagnosis and surgical treatment. Surgery should be performed as soon as possible before signs of liver cirrhosis develop.