Bacterial Meningitis Caused by Neisseria Meningitidis: An Overview
Bacterial meningitis caused by Neisseria meningitidis primarily affects children. This disease develops due to purulent inflammation in the meninges, where the bacteria can invade through the bloodstream or lymphatic system (bacteremia or true septicemia) from an infectious focus elsewhere in the body. The disease typically localizes in the meninges of the cranial dome.
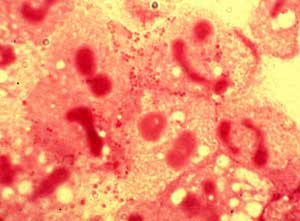 |
| Neisseria meningitidis (Image: ulb.ac) |
Meningococcal infection can manifest as nasopharyngitis, bacteremia, or meningitis. This illness is common in our country and has the potential to spread in an epidemic form.
Symptoms and Manifestations
The symptoms vary depending on the form of the disease.
Upper Respiratory Tract Form (nose, throat): Sudden high fever of 38-39°C, headache, sore throat, runny nose (clear or purulent). The fever lasts for 5-7 days. Examination reveals hyperemia and significant edema of the tonsils, pharynx, and nasal mucosa. This benign illness lasts only 5-7 days and is often confused with other bacterial infections like those caused by Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis. If detected early and treated promptly, the disease can be cured.
Bacteremia Form: This can be simple bacteremia or may present as an acute form.
The simple bacteremia caused by Neisseria meningitidis presents with a high fever of 40-41°C, which may be continuous or intermittent, accompanied by chills, headache, and generalized muscle and joint pain. After the fever, a rash may appear. The rash is a very significant diagnostic indicator, which can be either simple petechiae or petechiae with necrosis. The rash typically appears 5 to 15 hours after the onset of fever. It may be widespread but is most commonly seen at the fingertips and toes. The rashes vary in size and may appear in different stages on the same area of skin. As the disease worsens, the rashes may become necrotic, and there may be enlargement of the liver and spleen. Blood pressure may drop in cases of shock.
Acute bacteremia due to Neisseria meningitidis manifests with bacteremia and shock due to the toxins of the bacteria: hypotension, rapid and weak pulse, low temperature (below 36°C), decreased urine output or anuria. Rashes appear early accompanied by severe necrosis, sometimes with internal bleeding. If not detected early and treated promptly, the condition worsens and has a very poor prognosis.
Typical Meningitis Form: This form appears after upper respiratory infections or bacteremia or may occur immediately, presenting with two characteristic syndromes:
- Infectious and Toxic Syndrome: Sudden high fever of 39-40°C, continuous fever or fever in two phases. Fatigue and severe headache.
- Meningeal Syndrome: Typically appears early with prominent symptoms such as severe headache, gastrointestinal disturbances (projectile vomiting, constipation). The patient may lie in a gun position with signs of neck stiffness, Kernig’s sign, meningeal irritation, and photophobia, often turning their face to the wall.
In addition to the typical meningitis form, an acute meningitis-encephalitis form may also occur, characterized by high fever, agitation, restlessness, seizures, and coma. The pulse may slow, blood pressure fluctuates, and there may be severe respiratory disturbances. In this case, if not treated promptly, the prognosis is very poor.
Cerebrospinal Fluid Analysis is Necessary: In the typical meningitis form, intracranial pressure is elevated, cerebrospinal fluid is turbid (in mild cases, it may be clear), protein levels are increased while glucose and sodium chloride levels are decreased. A Gram stain reveals more than three white blood cells in a single field (usually the white blood cell count is very high). Gram staining shows coffee bean-shaped diplococci (Gram-negative), present both inside and outside the white blood cells. If conditions allow, culturing the bacteria can help identify Neisseria meningitidis based on biological properties and specific serological agglutination tests.
Prevention and Treatment
To prevent meningococcal meningitis, personal hygiene is essential, especially daily oral and throat hygiene. Patients should be isolated, and contact with infected individuals should be avoided, as the bacteria can spread through respiratory droplets and mucous from coughing or speaking, which can be inhaled directly by healthy individuals nearby. Currently, there is a specific vaccine available, and children under 36 months should be vaccinated to induce active immunity.
In cases of meningococcal infection, bacterial isolation and sensitivity testing to antibiotics should be conducted. Based on the antibiotic susceptibility results, appropriate antibiotics should be selected for treatment. In facilities where bacterial isolation and sensitivity testing are not available, treatment should be based on established protocols.
Currently, during hot weather, the disease can spread easily, so mothers should educate themselves about the disease to protect their children.


















































