The University of Texas at El Paso (UTEP) has developed a rapid cancer detection device that delivers results in just one hour at a cost of only $3, although more research time is needed for regulatory approval.
The research was published in the journal Lab on a Chip at the end of October. Experts at the University of Texas (UTEP) have developed a cancer traceability system in blood that is more sensitive than current diagnostic methods.
The device, named PiPP (paper-in-polymer-pond), costs approximately 70,000 VND (3 USD) and has a simple structure consisting of a filter paper stretched over a plastic frame. It is likened to “coffee filter,” promising to make cancer detection quicker, more accessible, and affordable.
With just a drop of the patient’s blood, PiPP targets two cancer markers: carcinoembryonic antigen (CEA) related to colorectal cancer and prostate-specific antigen (PSA) that warns of prostate cancer.
CEA and PSA appear in the blood in the early stages of the disease, making them difficult to detect using traditional methods. However, the new device can indicate these markers at low concentrations, being approximately 10 times more sensitive than existing test kits on the market.
“The biochip device is low-cost – just a few dollars – and highly sensitive. This will help many people receive accurate diagnoses more easily, regardless of their economic conditions”, said Professor XiuJun Li, a chemistry and biochemistry expert at UTEP and the lead author of the study.
Mr. Li added that PiPP is portable, providing quick results without the need for specialized instruments. The device can detect colorectal cancer at an early stage, giving results quickly, in just one hour, shorter than the 16 hours required for traditional tests. Users can also read the results on their smartphones.
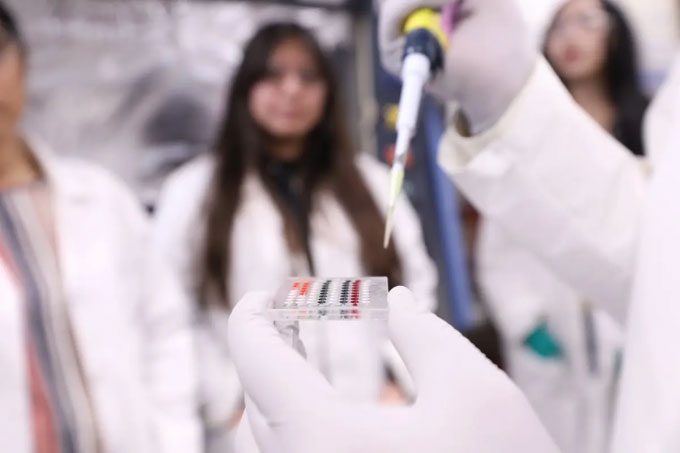
The PiPP device helps diagnose cancer quickly and easily. (Photo: The University of Texas at El Paso)
Experts note that people in poorer countries often lack access to cancer screening methods and resources. This limitation hinders early detection and treatment, leading to higher mortality rates. PiPP can be reused and is user-friendly, bridging gaps in cancer diagnosis worldwide.
According to Dr. Robert Kirken, Chair of the Department of Science at UTEP, PiPP enhances onsite screening capabilities, making it suitable for areas with limited resources.
Despite its potential, PiPP may require several years to commercialize. Scientists will conduct clinical trials to assess the device’s effectiveness and safety before submitting an application to the U.S. Food and Drug Administration. If approved, they plan to provide it to hospitals and clinics. The device promises to diagnose colorectal and prostate cancers.
Colorectal cancer has been increasing steadily among adults under 50 since the 1990s. Young people diagnosed with colorectal cancer are often identified at later stages of the disease when the tumor has become malignant. PiPP could serve as an early detection tool, improving prognosis.
Prostate cancer is also part of the “cancer pandemic” that is spreading. 10% of new cases in the U.S. occur in men under 55. The number of deaths due to prostate cancer is projected to increase by 136% from 2022 to 2050 globally. Like all cancers, early detection is crucial. PiPP could be a game-changer.


















































