Hypercholesterolemia, also known as lipid disorder, is commonly referred to as blood fat disorder (BFD) by many people. This condition is quite prevalent and is a concern for many. BFD is a major risk factor for several serious diseases such as atherosclerosis, coronary artery disease, and cerebrovascular accidents.
What is a blood fat disorder?
 |
|
(Image: VTC) |
Blood fat primarily exists in two forms: cholesterol and triglycerides. BFD is a condition characterized by an increase in harmful lipids and a decrease in beneficial lipids that protect the body. For cholesterol and triglycerides to circulate in the body, they combine with substances known as low-density lipoprotein (LDL), high-density lipoprotein (HDL), and very low-density lipoprotein (VLDL). LDL and HDL are responsible for transporting cholesterol, while VLDL transports triglycerides in the blood. Most cholesterol in the body exists in the form combined with LDL (denoted as LDL-c), with only about 1/4 to 1/3 combined with HDL (denoted HDL-c). Excess LDL-c can lead to the formation of atherosclerotic plaques, which is why it is colloquially referred to as “bad cholesterol.” HDL-c, on the other hand, is beneficial for the body as it counters the atherosclerosis process by transporting excess cholesterol accumulated in blood vessel walls back to the liver, thus earning it the title of “good cholesterol.” Elevated levels of triglycerides in the blood also contribute to the atherosclerosis process. There is a constant balance between these two harmful and protective processes in our bodies. When we refer to BFD, it means an increase in harmful components and a decrease in protective beneficial components.
What are the dangers of blood fat disorders?
 |
| (Image: VTC) |
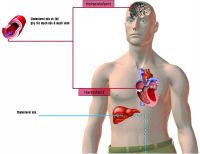
Several factors affect cholesterol levels in the blood. Numerous studies on BFD worldwide indicate that when total cholesterol exceeds 240 mg%, the risk of coronary artery disease increases by 2-3 times. High levels of “bad” cholesterol (LDL-c) in the blood elevate the risk of myocardial infarction. Conversely, low levels of “good” cholesterol (HDL-c) increase the risk of cerebrovascular accidents and atherosclerosis. Moreover, elevated triglycerides are particularly common in patients with diabetes, who also face a higher risk of atherosclerosis.
If LDL-c is high but HDL-c is also elevated, there is less cause for concern compared to a situation where LDL-c is high and HDL-c is low. BFD does not cause immediate harm, but its long-term effects can be very dangerous. Medical research has demonstrated that effectively addressing BFD is essential to limit coronary artery events, cerebrovascular incidents, and to reduce mortality rates from vascular complications.
Treatment and Prevention
People with BFD should not panic or be overly anxious. Instead, they should calmly implement a non-pharmacological treatment approach, which includes two basic elements:
Dietary restrictions: Reduce the intake of saturated fats (animal fats, butter, coconut oil, etc.). If complete avoidance is not possible, limit saturated fats to no more than 1/3 of daily fat requirements. Decrease consumption of foods high in cholesterol such as organ meats (brain, kidneys, heart, liver, etc.). While egg yolks are high in cholesterol, they also contain a substantial amount of lecithin, which regulates cholesterol metabolism in the body. Therefore, complete avoidance is not necessary; consuming 2-3 eggs a week is acceptable. For those who are overweight, weight loss is essential. It is advisable to eat plenty of fresh fruits and vegetables and to drink green tea. Limit alcohol consumption and avoid smoking, as these can accelerate the atherosclerosis process and increase “bad” cholesterol levels.
Physical exercise: Engage in exercise suitable for individual health, aiming for 30-45 minutes of moderate activity at least three times a week. Exercise will enhance the effectiveness of dietary changes.
If, after implementing these non-pharmacological measures for 4-6 months, there is still no improvement in the BFD condition—particularly if “bad” cholesterol (LDL-c) remains high—then medication to lower blood lipids may be necessary. The medication options include one of four groups: statins, fibrates, niacin, or resins. Medication should always be prescribed and monitored by a physician, as these drugs can also have various side effects, in addition to lowering blood lipids.