If you encounter someone suffering from heatstroke, take them to a shaded or air-conditioned area, cover them with a damp cloth, or sprinkle cool water on their body.
First Aid and Prevention of Heatstroke
Heatstroke (also known as heat shock) is the most severe form of heat injury and is a medical emergency. Heat shock can be fatal or cause damage to the brain and other vital organs in the body. It primarily affects individuals over 50, but it can also impact healthy young people.
Symptoms of Heatstroke
The hallmark symptom of heat shock is a core body temperature exceeding 40.5 degrees Celsius. Fainting may often be the first sign.
Other symptoms may include:
- Severe headache.
- Dizziness and lightheadedness.
- No sweating despite hot weather.
- Red, hot, and dry skin.
- Muscle weakness or cramps.
- Nausea and vomiting.
- Rapid heart rate, which may feel strong or weak.
- Rapid and shallow breathing.
- Behavioral changes such as confusion, disorientation, or stupor.
- Seizures.
- Coma.
Initial First Aid for Heatstroke Victims
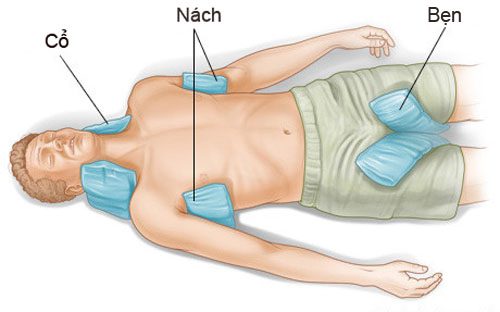
To cool down, apply ice packs to the armpits, groin, and neck of the heatstroke victim. (Photo: Examiner).
If you suspect someone is experiencing heatstroke, immediately call emergency number 115 or take the victim to the hospital. While waiting for medical assistance, move the patient to an air-conditioned place or at least a shaded area, and remove unnecessary clothing.
If possible, measure the patient’s body temperature and administer first aid to lower it to between 38.3-38.8 degrees Celsius. If a thermometer is not available, proceed with cooling methods immediately:
- Fan and wet the patient’s skin with a damp cloth or hose.
- Apply ice packs to the armpits, groin, neck, and back. These areas have many blood vessels close to the skin, so cooling them can help reduce body temperature.
- Immerse the patient in a cool shower or bath, or an ice bath.
If medical assistance is delayed, you can call the emergency room of a hospital for additional guidance.
A person who has recovered from heat shock may be more sensitive to high temperatures in the weeks following. Therefore, it is best to avoid hot weather and heavy exercise until a doctor confirms you are safe to return to normal activities.
Risk Factors for Heatstroke
Heat shock easily affects older adults living in environments without air conditioning or poorly ventilated homes. Other high-risk groups include individuals who do not drink enough water, have chronic illnesses, or consume excessive alcohol.
Heat shock is closely related to the heat index. The heat index is a measure of how hot it feels when humidity is combined with the air temperature. Humidity above 60% hinders sweat evaporation, thus impairing the body’s ability to cool itself.
The risk of heat-related disorders significantly increases when the heat index rises above 90 degrees. Therefore, it is crucial (especially during heatwaves) to pay attention to the reported heat index and remember that total exposure to sunlight can increase the reported heat index by 15 degrees.
If you live in an urban area, you may be especially vulnerable to heat shock during prolonged heatwaves, particularly if there is no breeze and poor air quality. The phenomenon of the “urban heat island effect” (asphalt and concrete buildings heat up during the day and slowly release heat at night) results in higher nighttime temperatures.
Other risk factors combined with heat-related conditions include:
- Age: Infants, children under 4 years, and adults over 65 are more vulnerable to heat as they adapt to heat more slowly than others.
- Health conditions: Heart, lung, or kidney diseases, obesity, underweight, hypertension, diabetes, mental illness, sickle cell disease, alcohol dependence, sunburn, and any condition causing fever… are all at greater risk of heat injury.
- Medications: The use of antihistamines, weight loss drugs, diuretics, sedatives, stimulants, anticonvulsants, cardiovascular and blood pressure medications, and psychiatric medications can increase the risk of heat injury. Drugs are also associated with an increased risk of heat shock.
However, individuals with diabetes—who are at higher risk of emergency care, hospitalization, and death due to heat-related disorders—often underestimate their risk during heatwaves.
Consult your doctor if you believe your health status and medications might affect your ability to cope with high temperatures and humidity (especially during heatwaves).

Working outdoors in high temperatures increases the risk of heatstroke. (Illustration: Quy Doan).
How to Prevent Heatstroke
When outdoor temperatures are high, it is best to stay in an air-conditioned environment. If you must go outside, you can take preventative measures against heat shock as follows:
- Wear loose, lightweight, light-colored clothing, a wide-brimmed hat, and use sunscreen with a sun protection factor above 30.
- Drink plenty of water to avoid dehydration, at least about 8 glasses of water, fruit juice, or vegetable juice… Since heat-related disorders can also result from salt loss, it is advisable to supplement with electrolyte-rich sports drinks during heatwaves.
Implement additional preventative measures when exercising or walking outdoors: drink about 710 ml of water two hours before exercising and consider adding a cup (about 240 ml) of water or sports drink just before exercising. During exercise, drink a cup of water every 20 minutes, even if you do not feel thirsty.
– Reschedule or cancel outdoor activities. If possible, change your outdoor time to cooler times of the day or early morning or after sunset.
Other heat shock prevention measures include:
- Monitor urine color: Darker urine is a sign of dehydration. Ensure you drink enough water to maintain clear urine.
- Weigh yourself before and after each physical activity. Monitoring weight loss can help determine how much water you need to replenish.
- Avoid caffeinated or alcoholic beverages as both can lead to increased fluid loss and exacerbate heat-related conditions. Additionally, do not take salt tablets without a doctor’s prescription. The easiest and safest way to replenish salt and other electrolytes during heatwaves is through sports drinks and fruit juices.
- Electrolyte abnormalities: In cases of dehydration, electrolyte imbalances may occur due to the loss of vital minerals (such as sodium, potassium, and chloride) from the body through sweat. For example, patients with diarrhea or excessive vomiting can lose significant amounts of potassium, leading to muscle weakness and arrhythmias.
- Consult your doctor before increasing your daily water intake if you have liver, kidney, heart, or seizure disorders (conditions that require water intake limitations) or have issues with fluid retention.
If your home lacks fans or air conditioning, during the hottest part of the day, consider going to an air-conditioned place (such as a supermarket, post office, bank, or even a neighbor’s house) or shaded areas. At home, close curtains, cover doors, or lower blinds during extreme heat and open windows on both sides of the house at night to create ventilation.
How to Prevent Dehydration in Hot Weather?
In reality, there is no standard amount of water that adults and children should drink daily. Hydration depends on body weight, climate, and more. Additionally, we need to choose appropriate foods for summer to keep our spirits and physical health in a healthy state, according to Everyday Health.
Drink a glass of water upon waking: After sleeping for 6-8 hours, the body wakes up in a dehydrated state. At this point, a glass of warm water helps detoxify the accumulated toxins and increases skin moisture.
Consume Hydrating Foods: Fruits such as strawberries and watermelon, as well as vegetables like lettuce, cabbage, celery, and spinach, contain about 90% water. Dairy products, including milk, yogurt, and cheese, are also abundant sources of hydration.
Drink Plenty of Water During Hot Weather and When Ill: In cases of children or adults with fever, diarrhea, or excessive vomiting, mild to moderate dehydration requires replenishment of fluids and electrolytes. Those working in hot environments or engaging in physical activities that cause sweating also need to replenish electrolytes and fluids as necessary.

Increase water intake and hydrating foods during summer.
Hydrate During Physical Activity: Drinking water during sports activities or hiking is essential. Runners should consume 30 ml of water about 2 hours before their run, along with a light snack. About 15 minutes before running, drink a cup of water.
If running for more than an hour, drink water regularly; the amount needed will vary based on your sweat rate. Those who sweat heavily may need 30 ml every 15 minutes. After running, make sure to hydrate, along with a light meal and fruits.
Protect Your Body from Sun Exposure: In the summer, with high temperatures, wear loose, light-colored clothing. Schedule strenuous physical activities during cooler parts of the day. Protect yourself from the sun with hats and sunglasses.
It’s important to note that dehydration does not occur rapidly, and correcting fluid deficits can take hours as electrolytes redistribute properly in different spaces within the body. Therefore, if rehydration is too slow, patients may experience prolonged low blood pressure and shock. Conversely, if done too quickly, the concentrations of water and electrolytes in organ cells may be negatively affected, leading to cell swelling and potential damage.


















































