In Ho Chi Minh City, the meningococcal meningitis situation is becoming increasingly complex. As of yesterday, Children’s Hospital No. 2 has had to provide preventive medication to staff and medical personnel who came into contact with patients.
 |
| Doctors at Children’s Hospital No. 2 (Ho Chi Minh City) are caring for and treating patient Thanh Mai. (Photo by VNN taken on March 23) |
In the early morning of March 20, Children’s Hospital No. 2 admitted a patient named Hoang Thi Thanh Mai, a 3-year-old girl from Binh Chieu, Thu Duc, presenting with high fever, lethargy, and vomiting.
Clinical examination and tests confirmed that the child was suffering from meningococcal meningitis.
Meningococcal Meningitis: 6 Cases, 3 Deaths, 2 Cases with Unknown Serotype
Thus, in recent weeks, Ho Chi Minh City has reported 6 cases of meningococcal infection, with 3 fatalities. All cases have been concentrated in Thu Duc District.
As of 4 PM on March 22, at the Infectious Diseases Department of Children’s Hospital No. 2, Thanh Mai remained in a state of lethargy, despite being treated with strong antibiotics immediately after diagnosis. Although her fever had decreased, she was still very weak and sluggish.
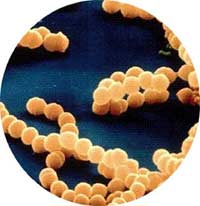
Dr. Tran Thi Viet, Head of the Infectious Diseases Department at Children’s Hospital No. 2, stated that purulent meningitis, also known as meningococcal disease, is caused by a type of bacteria that only affects humans.
Dr. Viet also indicated that Thanh Mai’s case was identified as being infected with serogroup C.
The two previously surviving cases in Thu Duc were infected with serogroup B.
As for the 2 out of 3 deceased cases, the serotype has not yet been determined.
Poor living conditions, overcrowding, and humidity are significant factors contributing to the outbreak. Evidence shows that recent cases have all originated from makeshift housing areas for workers. Anyone can contract the disease, but actual data indicates that the most susceptible age group is typically between 5 to 15 years old.
 |
| Bruises caused by meningococcal disease (Photo: thailabonline) |
This type of bacteria resides in the nose and throat of some individuals without causing illness (these are known as asymptomatic carriers), with an approximate rate of 10% among those living in well-ventilated environments. However, in cramped and poorly sanitized conditions, this rate is significantly higher. The disease tends to emerge when the body’s immune system is weakened or following a prior infection.
This disease was once very common, but its incidence has decreased significantly over the past 5 years due to the availability of vaccines.
Patients with the septicemic form of meningococcal disease account for only about 10-20% of cases, but the mortality rate is very high, around 50%, even with intensive resuscitation efforts. Survivors often require skin grafts due to deep tissue damage.
Interestingly, epidemiologists have not yet explained why individuals who are larger, healthier, and have strong immune systems, or infants who are well-nourished, are more susceptible to the severe forms of septicemia.
Among all the bacteria that cause meningitis, the one that causes meningococcal disease is the most contagious and spreads through respiratory secretions.
The onset of the disease is very sudden, without prolonged symptoms.
Therefore, parents should be vigilant if they notice that their child suddenly has a high fever, cough, sore throat (or sometimes no cough and sore throat), but also experiences vomiting. Additionally, if red or purple spots appear on the skin or bleeding in the eyes within a short period, the child should be taken to the hospital immediately without self-medicating.
Upon admission, the child will undergo immediate blood tests, and if there are signs suggestive of meningitis, a cerebrospinal fluid test will be conducted.
Vaccination: Currently Only 2 Serotypes Are Preventable
To protect healthcare workers who come into contact with children, starting from the afternoon of March 23, Children’s Hospital No. 2 organized for all staff in the Infectious Diseases Department and those who had initial contact with the patient to take a single dose of a preventive medication called Ofloxacin 400mg.
Currently, there is a meningococcal vaccine available, but it only protects against serogroups A and C, while serogroups B and D remain unvaccinated.
The disease is most contagious during the first 24-48 hours after the onset of symptoms.
According to doctors at Children’s Hospital No. 2, if possible, infected children should be isolated. However, due to the limited space in the Infectious Diseases Department, children with other illnesses still have to share a room with those diagnosed with meningococcal disease.
When infected, if in the mildest form, the patient may only experience a sore throat and can recover on their own. In more severe cases, there are two clinical presentations: – If the bacteria enter the bloodstream, causing septicemia: the patient does not have meningitis, but this does not mean it is not dangerous. In severe cases, the patient can die very quickly within 24-48 hours, with a mortality rate of up to 50%. If they survive, they may require skin grafts due to necrotic skin. The two recent fatalities in Tam Binh, Thu Duc, were also due to meningococcal septicemia. When infected with meningococcal disease, symptoms may include cough, sore throat, fever, chills, muscle pain, coma, shock, and purpuric spots on the skin (which can appear as dark purple, red, and vary in size, leading to necrosis). |
Nhật Phương