A trial HIV vaccine based on mRNA technology, the same technology behind two highly effective Covid-19 vaccines, has shown promising results in mice and primates.
Research results published in the journal Nature Medicine on December 9 by scientists at the National Institute of Allergy and Infectious Diseases (NIAID) indicate that the new vaccine is safe, generates antibodies, and elicits immune responses in cells against HIV-like viruses. Macaques that received the initial vaccine dose, followed by several booster shots, had a 79% lower risk of exposure to the simian immunodeficiency virus (SHIV) compared to unvaccinated animals. The study was conducted by Dr. Paolo Lusso at the Immunology Monitoring Laboratory of NIAID, along with several scientists from the same institute and Moderna.
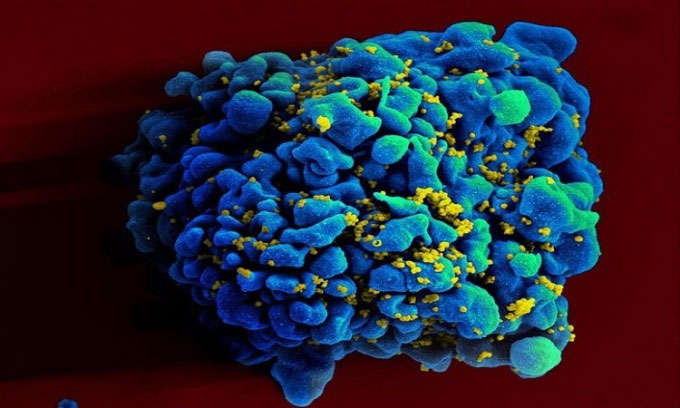
Electron microscope image of T cells H9 infected with HIV. (Photo: NIAID)
“Despite the efforts of the global research community for nearly four decades, an effective vaccine to prevent HIV remains a distant goal,” said Anthony S. Fauci, director of NIAID and co-author of the study. “This experimental mRNA vaccine incorporates several features that may address many limitations of other experimental HIV vaccines, making it a promising approach.”
The new vaccine functions similarly to the Covid-19 mRNA vaccines. However, instead of encoding information for the spike protein of the novel coronavirus, this vaccine provides information to produce two key HIV proteins: Env and Gag. Muscle cells in the vaccinated animals assemble these two proteins to create virus-like particles (VLP) with multiple copies of Env on their surface. Although they cannot cause infection due to the lack of complete HIV genetic material, these VLPs closely mimic HIV in terms of stimulating the appropriate immune response.
In studies with mice, two doses of the mRNA vaccine produced neutralizing antibodies in every animal. The Env protein produced in the mice from the mRNA information closely resembles the protein in the complete virus. This is a significant improvement over previous experimental HIV vaccines. According to Dr. Lusso, the presence of multiple copies of the HIV capsid protein in each VLP is one of the unique features that closely simulates the natural infection mechanism, potentially contributing to the desired immune response.
The research team continues to test the Env-Gag VLP mRNA vaccine in macaques. The vaccine doses differ among groups of monkeys but all include an initial dose and several booster shots over a year. The booster vaccine contains Gag mRNA and Env mRNA from two groups of HIV viruses instead of one as in the initial shot. The team uses various viral strains to stimulate antibody activation.
Despite the relatively high mRNA vaccine doses, the product only caused very mild temporary side effects in the macaques, such as a loss of taste. By week 58, all vaccinated monkeys developed neutralizing antibody concentrations targeting the most common strains among the 12 HIV strains used in the trial. In addition to antibodies, the mRNA VLP vaccine also produced a strong T-cell response.
Starting week 60, the vaccinated animals were immune, and a group of unvaccinated macaques was exposed weekly to SHIV through rectal mucosa. Since primates are not affected by the HIV-1 strain, scientists used a hybrid SHIV in the experiment, as that virus replicates in macaques. After 13 weeks of vaccination, 2 out of 7 immunized monkeys were not affected by the virus. The remaining animals were infected more slowly (averaging 8 weeks). In contrast, unvaccinated animals became infected on average after 3 weeks.
“We are improving the vaccine to enhance the quality and quantity of VLPs. This could increase the vaccine’s efficacy, thereby reducing the number of doses needed to elicit a strong immune response. If confirmed safe and effective, we plan to test the vaccine in a Phase 1 trial in healthy adult volunteers,” Dr. Lusso shared.


















































