Botulinum poisoning is typically diagnosed through the analysis of stool samples and vomit, and treated with antitoxin medications, antibiotics, or ventilatory support.
Botulinum is an extremely potent neurotoxin that can cause muscle paralysis, respiratory distress, or death with as little as 0.004 μg/kg. The most recent high-profile case of alleged botulinum poisoning involved American student Otto Warmbier, who became paralyzed while in North Korea and subsequently died at home.
Initial symptoms include fatigue, weakness, and noticeable dizziness. Patients often display blurred vision, dry mouth, difficulty swallowing, and trouble speaking. Some cases may experience vomiting, diarrhea, constipation, and abdominal bloating.
If not treated promptly, the illness may progress to muscle weakness, particularly in the arms. Following this, the respiratory organs and lower body may be affected. Individuals suffering from botulinum poisoning do not typically experience fever or loss of consciousness.
Symptoms usually appear within 12 to 36 hours (with a minimum and maximum range of 4 hours to 8 days) after exposure to contaminated food. The incidence of poisoning is low, but the risk of death after infection is quite high if not treated promptly and appropriately. The mortality rate after poisoning is between 5-10%.
To diagnose botulinum poisoning, doctors will check for signs of muscle weakness or paralysis, such as drooping eyelids and slurred speech. Patients may also be asked to list the types of food they have consumed over the past week.
In cases of infant poisoning, it is often due to exposure after consuming honey, presenting symptoms like constipation and lethargy.
Blood, stool, or vomit analysis may also assist in diagnosing botulinum poisoning. However, these tests typically take several days, so clinical examination is prioritized.
In some cases, patients may be referred for an electrocardiogram, MRI to check for signs of stroke, or a spinal tap to differentiate from a similar syndrome known as Guillain-Barre.
For botulinum poisoning cases, doctors will treat by emptying the digestive system, inducing vomiting or frequent urination. In cases involving wound contamination, surgery to remove infected tissue may be performed, depending on the severity.
One of the fundamental treatments for those diagnosed early is the administration of antitoxin, which reduces the risk of complications. The medication will bind to the toxins still circulating in the blood, preventing them from “running” into the nervous system.
This measure cannot completely reverse the initial damage caused by botulinum. However, nerves have a self-repair mechanism. Many patients recover fully, while some may take several months for treatment.
In Vietnam, Bach Mai Hospital has proposed purchasing antitoxin from Thailand to treat a couple suffering from botulinum poisoning. The medication, known as Botulism Antitoxin Heptavalent, is being expedited with support from the Ministry of Health and the World Health Organization (WHO) for timely treatment.
|
What is special about Botulinum Antitoxin? Dr. Nguyen Trung Nguyen, Director of the Poison Control Center, stated that this medication, called Botulism Antitoxin Heptavalent (BAT), is produced in Canada and is specifically used to treat botulinum toxicity. According to the U.S. Food and Drug Administration, BAT is a mixture of antibodies labeled A, B, C, D, E, F, G that specifically treat the various forms of botulinum toxin. Mechanistically, BAT provides passive immune response for the body through the antibodies it possesses. Specifically, when injected into a person, these antibodies tightly bind to free botulinum, preventing them from interacting with the receptors of nerve cells. Through this mechanism, BAT significantly reduces paralysis and muscle weakness in patients with botulinum poisoning. Patients receiving detoxification will have a reduced risk of severe complications requiring mechanical ventilation. |
For infants, doctors worldwide often use a specific antitoxin known as human immunoglobulin.
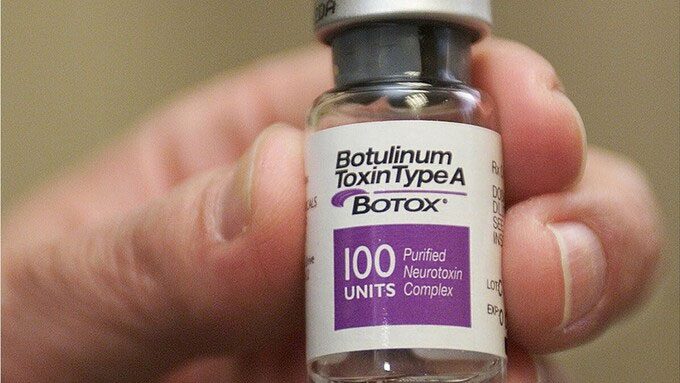
One of the medications used to treat botulinum poisoning. (Photo: AP).
In some cases, patients may be prescribed antibiotics. However, this method is not recommended for all types of botulinum poisoning, as it may accelerate the spread of toxins.
If experiencing difficulty breathing, patients may require ventilatory support for several weeks until the effects of the toxin diminish. This process may take weeks or even months.
After detoxifying, some patients may need rehabilitation therapies to improve their speaking, swallowing, and affected bodily functions.
To prevent botulinum poisoning, individuals should adhere to the principle of “cooking thoroughly and boiling water.” Some heat-sterilized products in industrial and commercial chains (including vacuum-packed or smoked items) may not meet hygiene standards and fail to eliminate all bacterial spores.
WHO has previously outlined Five Keys to Food Safety: keep clean, cook thoroughly, separate raw and cooked foods, store food at safe temperatures, and use safe water and ingredients.
According to WHO, mass outbreaks of botulinum poisoning are very rare but constitute public health emergencies that require rapid recognition to identify the source of illness. Patient prognosis significantly depends on early diagnosis and appropriate treatment.
Although botulinum poisoning can cause severe and prolonged symptoms, most affected individuals recover fully. Early treatment helps reduce the risk of death or permanent disability.


















































