 Life, in conventional terms, is the result of the activities of various organs and internal systems within the body working to maintain and develop each individual. In other words, living means resisting death.
Life, in conventional terms, is the result of the activities of various organs and internal systems within the body working to maintain and develop each individual. In other words, living means resisting death.
From a legal perspective, most countries around the world recognize the status of a human being for their citizens beginning at birth and ending with that individual’s death. Medicine considers individuals who attempt suicide or have suicidal intentions to be experiencing a mental disorder, even if only momentarily.
When is a person considered dead?
Everyone has the right to live, a right that is absolutely protected by the constitutions of each country, except in certain special cases, such as when a mother must terminate a pregnancy for her own health.
The definition and accurate diagnosis of human death holds significant importance. To avoid committing homicide, even unintentionally, the burial of the deceased and the retrieval of organs for transplantation can only be performed on individuals deemed to be dead. The sensitive and complex issue is determining at what point a person is considered dead and what methods are used to diagnose death.
Human death is often simply defined as the permanent cessation of life signs, specifically the heart stopping and breathing ceasing. The invention of the stethoscope in the 19th century and the electrocardiogram in the 20th century has enabled accurate confirmation of the heart’s cessation.
However, today, with the invention of ventilators and pacemakers, the signs of death have become ambiguous, prompting clinical and forensic medical professionals to suggest that the relationship between the functions of the respiratory, cardiovascular, and central nervous systems should be used to determine the boundary of death.
Is death brain death?
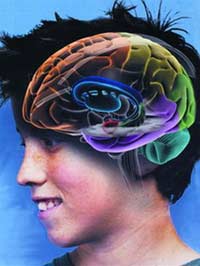
According to new standards based on advances in biomedical science, a person is considered dead when all brain activity ceases irreversibly. In clinical practice, brain death typically results from two main causes: severe brain injury or hemorrhage, which are less common.
In contrast, the cause of cardiac arrest interrupts blood supply to the brain, leading to severe cerebral ischemia, which is the more common cause of complete brain death, occurring in many diseases and various instances of cardiac arrest.
Thus, the interdependence of the three systems—the respiratory, circulatory, and central nervous systems—has been confirmed in all genuine circumstances of human death. The general standards for death are unified worldwide, as stated by author Byrne: “No one should be declared dead until there is destruction of at least three essential systems in the body: the brain, cardiovascular, and respiratory systems.”
Therefore, in the medical field, in addition to detailing the clinical signs deemed necessary to conclude that a patient is dead, there are also stringent regulations, such as the requirement for reevaluation until the diagnosis of the patient’s permanent departure is established. In Sweden, a person may only be considered dead after intensive resuscitation for 30 minutes or irreversible coma lasting from 6 to 48 hours, depending on the cause and age. In Germany, a physician may only confirm death after the neurological, circulatory, and respiratory functions have been irreversibly absent for more than 3 hours.
When a patient is on a ventilator or connected to a pacemaker to sustain lung and heart function, brain death criteria must be applied to definitively diagnose that the patient has passed away. Diagnosing brain death is straightforward with the aid of an electroencephalogram, where the absence of characteristic brain activity waves—alpha, beta, or delta waves—results in a flat line throughout the measurement process.
The transition from life to death is a dynamic process and does not occur instantaneously, especially under the remarkable advancements in medicine today. Patients are continuously supported by various medications and machines. Therefore, it is challenging to assert exactly when life ceases and when a patient begins to die.
From a legal standpoint, there is only one death, which must be the same for everyone and in every situation. Conversely, the procedures for confirming a patient’s death may vary depending on circumstances, particularly regarding the family’s and medical professionals’ decisions on whether to retrieve organs for transplantation.
The brain plays a crucial role in maintaining the unity of the nervous system, and brain tissue is the most sensitive to oxygen deprivation. In reality, just 5 minutes of oxygen deprivation can lead to permanent brain tissue death, rendering it incapable of recovery. Thus, whether a patient dies from respiratory failure or cardiac arrest, it also results in the death of brain cells. In some cases, even if the brain is dead, the heart and lungs may still be functioning, providing blood to organs such as the kidneys, liver, and corneas, making the use of these organs for transplantation highly beneficial.
In general, the criteria for brain death in confirming an individual’s death is an inevitable result of advancements in scientific and technical understanding, representing progress in death diagnostics rather than a new definition of death. In other words, brain death is not a different kind of death.
There are two causes leading to death
Among the two causes of death, cases of brain death are significantly lower compared to those dying from cardiac arrest. According to data from emergency centers in the United States, up to 92% of patients die from cardiac arrest, while only 8% die from brain injuries.
The determination of brain death today in many developing countries, such as Vietnam, primarily serves to inform physicians and the patient’s family regarding when they have the right to cease supportive treatment and medications. In practice, due to the absence of laws on organ transplantation, very few cases are related to organ retrieval for transplantation. Retrieving organs when the brain is dead but the heart is still beating is ideal for transplant surgery.
Cases of cardiac death, to date, remain largely unsuitable for organ transplantation. The viability of internal organs, particularly those sensitive to oxygen deprivation, such as the kidneys and corneas, diminishes rapidly when blood supply ceases.
Assoc. Prof. Dr. NGUYEN HOAI NAM