The term fatty liver immediately brings to mind obesity or a diet rich in fats. In fact, malnutrition can also lead to this condition.
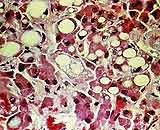 |
Cross-section image of a fatty liver showing white spots. (Photo: SK & ĐS) |
Among the causes of fatty liver are obesity, excessive alcohol consumption, and infection with hepatitis viruses. However, poor nutrition can also lead to fatty liver disease. A deficiency in substances that reduce fat metabolism in the liver or impede the function of fatty acids can cause the accumulation of fat and fatty acids in the liver, resulting in fatty liver disease.
When the body remains in a prolonged state of starvation (often seen in those who excessively diet), blood sugar levels become too low, increasing the sympathetic nervous system’s stimulation to absorb energy by breaking down fats. During this process, the excessive release of fatty acids into the bloodstream results in an increase in free fatty acids, leading to fat accumulation in the liver.
A long-term deficiency in protein hampers the formation of apoproteins, causing blood fats to be unable to metabolize in a timely manner, which results in increased blood fats—a crucial condition for the development of fatty liver.
A deficiency of certain vitamins and inorganic salts also hinders fat metabolism, causing fatty liver disease. Irregular nutrient intake can lead to a lack of amino acids necessary for the transport of fats, preventing the timely movement of triglycerides in liver cells and resulting in fatty liver disease.
Fatty liver is mostly chronic, and mild cases may not present any clinical symptoms. In moderate to severe cases, symptoms may include: loss of appetite, nausea, vomiting, and abdominal distension. Some individuals may also exhibit vitamin deficiency symptoms that cause neuritis, cheilitis, skin bruising, keratosis of the skin, nails, and hair… Those in severe cases may experience jaundice and ascites. Without treatment, complications such as cirrhosis and liver cancer may occur.
Once the cause of fatty liver due to malnutrition is identified, doctors will determine the appropriate treatment based on the severity—mild, moderate, or severe. Mild and moderate cases are usually treated with dietary changes and intravenous medication. Dietary recommendations include a focus on high energy, protein, vitamins, and fiber intake.
Due to long-term malnutrition, digestive system function decreases, so when supplementing nutrients from plant sources, it must be based on the body’s absorption capacity. If necessary, digestive enzymes such as insulinase may be supplemented. When increasing protein intake, the quality of the protein should be considered; foods such as meat, fish, beef, goat meat, and various types of eggs are recommended.
It is advisable to avoid excessive fat intake. Only the necessary amounts should be supplemented. For those with severe malnutrition and poor absorption and digestive function, it’s best to consume low-fat foods initially, increasing fat intake only after digestive function returns to normal. Additionally, based on the condition, treatment may include nutritional components such as intravenous amino acids and vitamins…
To prevent the disease, one should not rely on a single type of food to avoid malnutrition. Avoid blindly fasting for weight loss, as this can lead to a loss of appetite, a condition that can contribute to fatty liver disease. A scientific approach to weight loss should combine proper diet with suitable physical activity to gradually reduce fat; losing 5 kg per month significantly increases the risk of fatty liver.
For individuals suffering from gastrointestinal ulcers, dementia, chronic digestive diseases…, timely and proactive treatment and nutritional adjustments are essential to avoid malnutrition or dietary imbalances that may lead to fatty liver disease. Special attention should be paid to the risk of malnutrition in children during weaning; it is crucial to supplement their diet, particularly with protein.
Dr. Trần Quốc Minh

















































