In recent years, rabies appears to be on the rise in Vietnam, particularly in Phu Yen province. According to reports from the Phu Yen preventive medicine center, in the first quarter of 2018, 1,639 people were treated for dog bites at healthcare facilities, which marks an increase of over 42% compared to the same period last year. In 2017, there were 5,250 cases of dog and cat bites requiring rabies vaccinations, and unfortunately, two people died due to neglecting vaccination and receiving no treatment once the disease manifested.
Let’s take a closer look at what rabies is, its impacts, and the official recommendations from the Department of Preventive Medicine, Ministry of Health regarding preventive measures against rabies.
First, here are some statistics compiled by the CDC regarding rabies in Vietnam. Over the past ten years, Vietnam has reported a total of 914 human rabies fatalities, averaging approximately 91 deaths per year. Similar to many other countries in Asia, Vietnam has a low vaccination rate for dogs, with many being allowed to roam freely without supervision. This leads to a higher likelihood of dog bites among people and increases the costs associated with post-exposure prophylaxis (PEP). According to CDC calculations, vaccinating one dog costs only $1.32, while a course of PEP can cost $153—nearly 116 times more. Studies have indicated that vaccinating 7 out of 10 dogs in a population can sufficiently protect the community.
Rabies is a disease caused by a type of virus that is transmitted from animals to humans. There are two clinical forms of rabies: the furious form and the paralytic form, with the furious form being the most common.
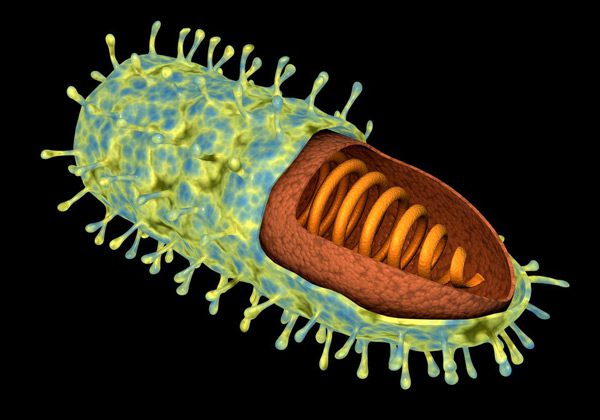
Rabies Virus.
Methods of Transmission of the Rabies Virus
The rabies virus enters the nervous system of mammals. It is primarily transmitted through the saliva of rabid animals to humans via bites or scratches on the human body. Rabies can also spread to humans when a rabid animal licks an open wound or comes into contact with scratched skin or the mucous membranes of the mouth or nose.
In Southeast Asia, 96% of rabies cases in humans are attributed to dog bites; however, there have been reports of rabies cases in humans due to bites from cats, civets, wild dogs, foxes, wolves, and other carnivorous animals. Rabies transmitted by monkeys and rodents is extremely rare. Horses and donkeys may become aggressive and bite hard when infected with rabies. Cattle and buffalo do not bite when infected, but precautions should be taken when examining sick animals exhibiting symptoms such as excessive salivation.
Sometimes, livestock owners confuse rabies with foot-and-mouth disease, septicemia with hemorrhage, or respiratory distress, leading to potential rabies virus exposure when they care for or administer medication to their pets by hand.
There have been no evidence-based reports of rabies transmission to humans through milk consumption. However, professional slaughterers may be at risk when handling the brains or other infected parts of rabid animals; still, there are no recorded cases of rabies transmission to humans from consuming well-cooked meat.
Transmission of rabies from person to person through corneal transplants or other organ transplants is relatively rare but possible. This type of transmission has occurred in corneal transplant recipients and recently in some solid organ transplant cases. Therefore, corneas or human body parts should not be sourced from patients who died from encephalitis or any other undiagnosed neurological diseases.
Although rabies patients rarely bite others, caregivers should exercise caution and remain vigilant when caring for rabies-infected patients, particularly avoiding contact with the patient’s saliva.

If a person is bitten by an animal, the following steps should be taken:
- Immediately wash the wound with soap and running water for about 10-15 minutes. If soap is not available, rinse the wound with clean water under running water for 15 minutes. This is the most effective first aid method against rabies.
- Thoroughly wash the wound with 70% alcohol or iodine solution, if available.
- Seek medical treatment at a healthcare facility as soon as possible.
Receiving post-exposure rabies vaccination (PEP) is mandatory if you are bitten by a rabid or suspected rabid dog, cat, or other animals. PEP should be applied under the following conditions:
- If the bite causes skin abrasions and bleeding.
- If mucous membranes come into contact with the saliva of a suspected rabid animal.
- If the animal has bitten a person:
+ It is dead.
+ It goes missing during observation.
+ It shows abnormal, erratic behavior.
+ If laboratory tests of brain material from the suspected rabid animal are positive.
The Department of Preventive Medicine, Ministry of Health recommends that the public follow these measures:
- Vaccinate 100% of pet dogs and cats and ensure yearly boosters as recommended by veterinary authorities.
- Keep dogs leashed or confined, and use muzzles when in public.
- Avoid teasing or provoking pets.
- If bitten by a dog or cat, immediately wash the wound under running water with soap for 15 minutes. If soap is unavailable, rinse directly with clean water. Avoid crushing the wound and do not bandage it tightly.
- Visit the nearest healthcare center for timely consultation and rabies vaccination.
- Absolutely do not self-medicate or seek treatment from unqualified practitioners for rabies.
The WHO also has a poster campaign about rabies, which you can view below:



















































