Penicillium marneffei Infection: A Critical Indicator of HIV Progression to AIDS
A 29-year-old male patient from Go Dau, Tay Ninh, was admitted to the Tropical Diseases Hospital in Ho Chi Minh City with a prolonged fever lasting approximately 30 days. Prior to this, he had been treated for malaria at Go Dau Hospital for about 10 days but did not see any improvement.
Early Death Due to Unidentified Fungal Infection
 |
| An AIDS patient with oral fungal infection. (Illustrative image) |
A few days later, the patient was transferred to Nguyen Trai Hospital in Ho Chi Minh City for an additional 10 days of treatment, yet the underlying cause of his illness remained unidentified, leading him to discharge himself from the hospital.
Three days after leaving, the patient was rushed back to the Tropical Diseases Hospital in a state of high fever, anemia, severe weight loss, and enlargement of the liver, spleen, and peripheral lymph nodes. The following day, he developed scattered papules on his face and genital area.
Blood culture tests revealed that the patient was infected with Penicillium marneffei (P.M) and also tested positive for HIV. Due to the previous medical facilities’ inability to identify the illness, the patient did not receive immediate antifungal treatment and unfortunately passed away before the fungal culture results were available.
Investigations showed that the patient had engaged in sexual relations with sex workers in Cambodia five years prior.
This case also marks the first documented instance of P.M infection in Vietnam, occurring 10 years ago.
P.M infection is not exclusive to AIDS patients; it also affects immunocompetent individuals. The severity of P.M infection varies depending on the level of immune system compromise. The infection rate is particularly high among AIDS patients—individuals with severely weakened immune systems.
Penicillium marneffei: A Sign of HIV Progression to AIDS
As many as 96.6% of P.M infections occur in AIDS patients. Once a patient reaches the AIDS stage, their immune system is severely damaged, creating an opportunity for P.M infection to thrive. Once infected, P.M impacts the immune system, exacerbating its already weakened state.
Research has shown that P.M is a critical indicator of AIDS. Since March 2005, the Ministry of Health in Vietnam has classified P.M infection as a diagnostic criterion for AIDS in HIV-infected individuals.
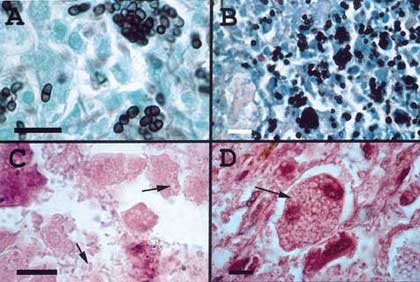
Image of Penicillium marneffei growth (Photo: Medscape)
Patients with systemic P.M infection typically present with symptoms such as prolonged fever, splenomegaly, leukopenia, anemia, persistent cough (sometimes with blood), and weight loss. Characteristic skin lesions include papules with central indurations that can sometimes lead to necrosis.
Dr. Nguyen The Dung noted that systemic P.M infection is a dangerous opportunistic infection that can lead to death if not treated promptly.
Untreated cases have a poor prognosis, with a mortality rate as high as 91.3% among non-AIDS patients and 100% among AIDS patients.
Even with treatment, the mortality rate remains significant, around 20%, because once P.M enters the body through the respiratory tract, it can subsequently invade the bloodstream and spread throughout the body, affecting various organs, including the skin and mucous membranes. The respiratory tract is the primary route of transmission. It is crucial to initiate antifungal treatment as soon as possible, starting with Amphotericin B, which can be combined with or replaced by Itraconazole.
Continuous antifungal therapy is vital as systemic P.M infection commonly occurs in patients with low CD4 counts and markedly impaired immune function. Notably, if preventive treatment is not maintained, the disease may relapse or result in death within a year.
To date, the Tropical Diseases Hospital in Ho Chi Minh City has identified and treated the highest number of P.M and HIV co-infected patients in the country, with 118 patients documented by the end of 2003. Notably, nearly half of these patients were unaware of their HIV status upon admission, leading them to seek care at other medical facilities with limited or no experience regarding this disease, complicating treatment.
Previously, this disease rarely appeared, resulting in limited experience, knowledge, and clinical awareness among doctors for detecting the illness. This led to missed or delayed diagnoses, impeding effective treatment. Research aims to help treating physicians recognize the disease more easily while establishing effective treatment protocols, which is the focus of Dr. Nguyen The Dung’s specialty graduation thesis.
Nhat Phuong


















































