The heart is one of the most important organs in the body. To better understand the inner workings of the heart, scientists have recreated the biological characteristics of this organ in a chip, a device the size of a credit card.
The “heart-on-a-chip” device has been newly developed by a research team from the National Institute of Standards and Technology (NIST) in the United States, simulating the interactions of human heart cells. Researchers state that this technology could be used to study heart disease, the leading cause of death in the U.S.
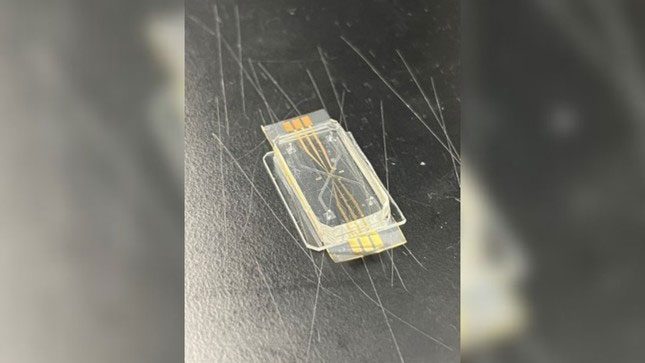
Heart-on-a-chip model captured in the laboratory. (Photo: Darwin Reyes-Hernandez and Derrick Butler/NIST).
Traditional experiments in mice and monkeys do not perfectly capture how diseases will progress or how drugs will function in the human body. Therefore, researchers are working to develop more accurate ways to simulate the complexities of human organs in the laboratory. This precision is particularly important for drug development, as 90% of candidate drugs currently fail in human clinical trials.
Heart-on-a-chip models
New models being developed include organs or organoids cultured from stem cells on a chip, where the cells are found to grow on a chip mimicking the organs in the human body. Many organs have been modeled in such chips, including the lungs, kidneys, and vagina.
In particular, scientists have developed heart-on-a-chip models to study how the heart heals after injury and disease, as well as to support drug research. “Heart-on-a-chip” has even been sent to space to study the effects of microgravity on the heart.
In a recent statement, the research team at NIST indicated that this technology, including their new heart-on-a-chip model, could streamline drug development, making it faster, safer, and more accurate. Importantly, these models cannot replace clinical trials in humans.
Darwin Reyes, a biomedical engineer at NIST and the lead developer of the new chip, stated: “This system could be considered for biomanufacturing and regenerative medicine for the heart and other organs on a chip.”
Development of human heart cells.
Chips containing hearts typically have a transparent or semi-transparent casing, and when viewed from the inside, researchers can observe fluids flowing through small interconnected channels like streams of water. In the case of the NIST chip, they simulated the blood vessels in the heart. Scientists develop human heart cells within it and can study how these cells respond to the addition of various drugs.
Reyes mentioned that, unlike existing heart-on-a-chip models, the cells in the new NIST model can be arranged so they can communicate with each other through molecules. He noted that the next step for the team is to assess how these heart cells function under normal conditions and stress-induced conditions.
Different organ chips can also be linked together – for example, a liver chip could be connected to a heart chip. This could allow scientists to investigate how these two organs interact after exposure to a specific drug.
In a recent review of these technologies published in the journal Lab on a Chip, Reyes and a colleague emphasized that several key tasks need to be completed before human organ models on a chip can be used in preclinical drug testing. For instance, the heart cells used in these devices are cultured from stem cells in a developing embryo.
The potential of these devices was recognized last year by the U.S. Food and Drug Administration, which ruled that they could replace traditional animal testing, provided their generated data is robust enough.




















































