A new study reveals that the cause of these auditory hallucinations lies in the brain’s inability to recognize its own speech signals. These findings may pave the way for treatment methods that go beyond medication, offering new hope to millions struggling with schizophrenia worldwide.
Schizophrenia, a complex mental disorder, often forces those affected to confront auditory hallucinations, specifically hearing voices that do not exist. These voices can be an overwhelming and persistent experience, significantly impacting the daily lives of those suffering from the condition.
Despite decades of research, the mystery surrounding why these hallucinations occur remains largely unsolved. However, a new study has provided groundbreaking discoveries that could open new avenues for treating schizophrenia without relying solely on medication.

Schizophrenia is a complex mental disorder.
Scientists have finally begun to understand the specific brain mechanisms that cause auditory hallucinations. This could change the way we think about the disorder and how we treat it.
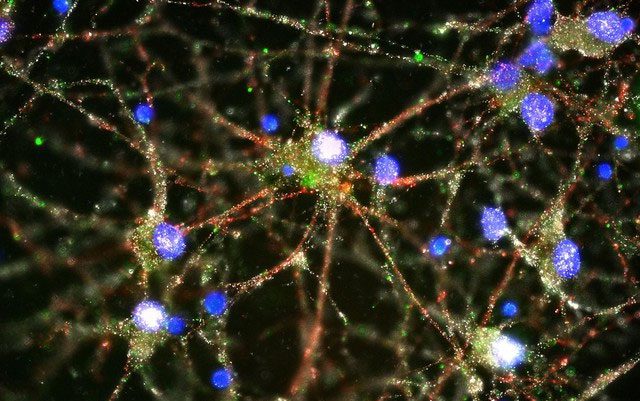
Researchers have long attempted to decode the brain mechanisms leading to auditory hallucinations in individuals with schizophrenia. Accordingly, a new study published in the journal PLOS Biology proposes a theory that the cause of these phantom voices may stem from the brain’s failure to recognize its own speech signals.
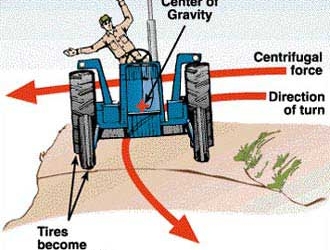
Typically, when a person prepares to speak, the brain generates a copy of the motor commands that control the mouth and tongue. This copy, known as “efferent copy,” is sent to the auditory system to indicate that the sound about to be produced comes from that person, not from an external source. However, in individuals with schizophrenia, this system appears to malfunction. Instead of recognizing their own voice, the brain processes it as a signal from the outside world, leading to auditory hallucinations.
The research team utilized electroencephalography (EEG) technology to analyze brain activity in three groups: a group of schizophrenia patients experiencing auditory hallucinations, a group of schizophrenia patients without hallucinations, and a control group of healthy individuals. Results indicated that both groups of schizophrenia patients had difficulty predicting their own voice sounds. However, in the group with auditory hallucinations, a more unusual occurrence transpired: the brain’s motor signals were excessive and flooded the auditory system, causing an internal sound disturbance that the brain could not accurately categorize.
According to Fuyin Yang, a neuroscientist at Shanghai Jiao Tong University and a co-author of the study, “Individuals with auditory hallucinations can ‘hear’ sounds without external stimulation. Poor functional connections between the motor and auditory systems are the reason they lose the ability to distinguish between real sounds and hallucinations.”
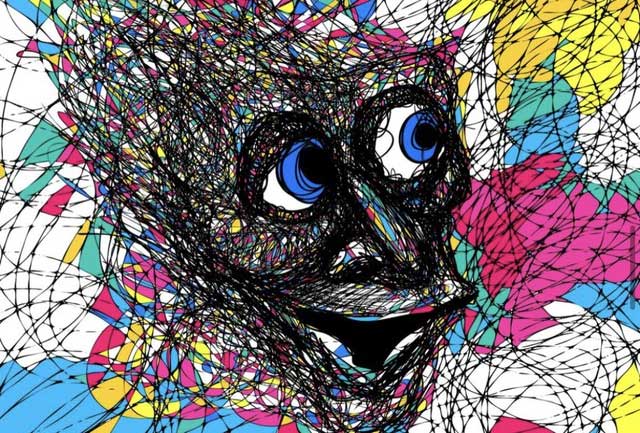
Individuals with auditory hallucinations can “hear” sounds without external stimulation.
The ability to recognize one’s own voice and suppress redundant signals is a process that we all undergo, albeit to a lesser degree. A simple example is the phenomenon of being unable to tickle oneself. Our brains have the capacity to predict the sensations when touching our own body, hence reducing the response when self-tickling. However, in individuals with schizophrenia, this internal inhibition does not function properly. As a result, their speech signals become uncontrollable, and the brain treats their own thoughts as if they were sounds from the outside.
This new study marks a significant advance in understanding how auditory hallucinations operate. For many years, scientists have identified disruptions in the brain’s motor system in individuals with schizophrenia, but it was unclear which signals were faulty. Thanks to this new research, we now have a more detailed insight into this process, which could lead to new treatment directions.
Tom Whitford, a psychology professor at the University of New South Wales in Australia, stated: “You cannot treat something that you do not fully understand. This finding provides specific insights into which aspect of the abnormal brain mechanisms in individuals with the disorder is at play.”
Currently, treatments for schizophrenia primarily rely on antipsychotic medications, but these can have severe side effects and may not be effective for everyone. For treatment-resistant patients, options become very limited. However, if faulty brain signals are the root cause of auditory hallucinations, non-invasive treatment methods such as transcranial magnetic stimulation (TMS) could be a solution.
The new study helps better understand how auditory hallucinations work.
Xing Tian, the lead author of the study and an associate professor of Neuroscience and Cognition at NYU Shanghai, shared: “Some patients find it very challenging to respond to medication. If our theory is correct, using a non-invasive neuromodulation technique could alleviate hallucination symptoms.”
This research comes at a crucial time as the FDA recently approved a new drug with the potential to change the treatment of schizophrenia. Combined with findings on the role of the brain in generating auditory hallucinations, the future of treating this condition may be much brighter than before.
With nearly 4 million people living with schizophrenia in the United States alone, scientific advancements like this bring hope that one day, the phantom voices in their heads may gradually fade away, leading to a more peaceful life.