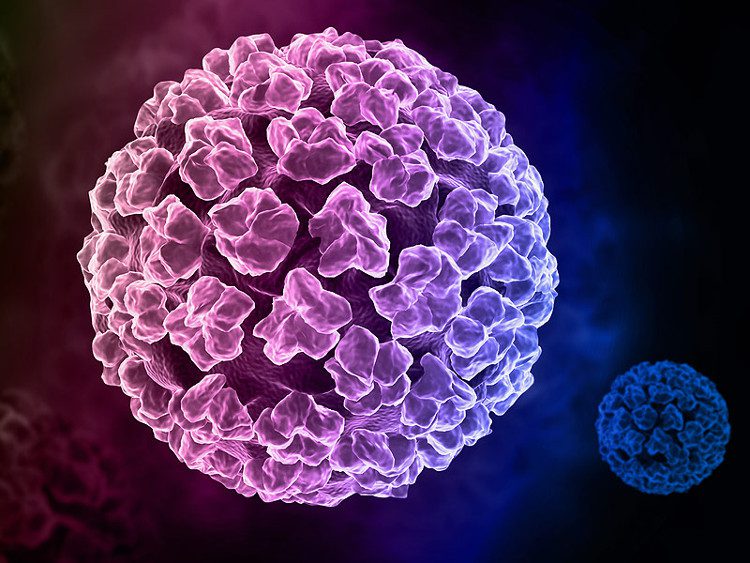
The incubation period for HPV is typically 3 weeks to 8 months from the time of infection until symptoms such as warts appear, primarily in the genital area.
According to Dr. Tra Anh Duy, genital warts, also known as condylomata acuminata or genital warts, commonly appear in the genital regions of both men and women due to the HPV virus. There are several causes of genital warts, which can be categorized into three groups:
- Unsafe sexual practices: The disease is transmitted through normal sexual intercourse, oral sex, and anal sex. Many people believe that oral sex poses no risk, but in reality, HPV can be found in the genital area, blood, saliva, and mucous secretions of infected individuals.
- Mother to child transmission: Women who have genital warts during pregnancy can transmit the virus to their fetus through the umbilical cord, amniotic fluid, or during labor. After the child is born, transmission may occur through contact with blood, vaginal fluids, or breastfeeding.
- The HPV virus can exist in the mucus secretions from warts, so intimate contact such as hugging, kissing, sharing personal items like toothbrushes, underwear, or bathing together can also lead to transmission. However, this type of transmission is relatively rare, accounting for a very small percentage of HPV infections.
Dr. Duy mentioned that the incubation period for genital warts typically ranges from 3 weeks to 8 months. The manifestations of genital warts can vary between men and women. Generally, early symptoms are more pronounced in men, which makes prompt treatment more effective. In women, the disease often progresses silently until it reaches a severe stage, at which point it is usually detected.
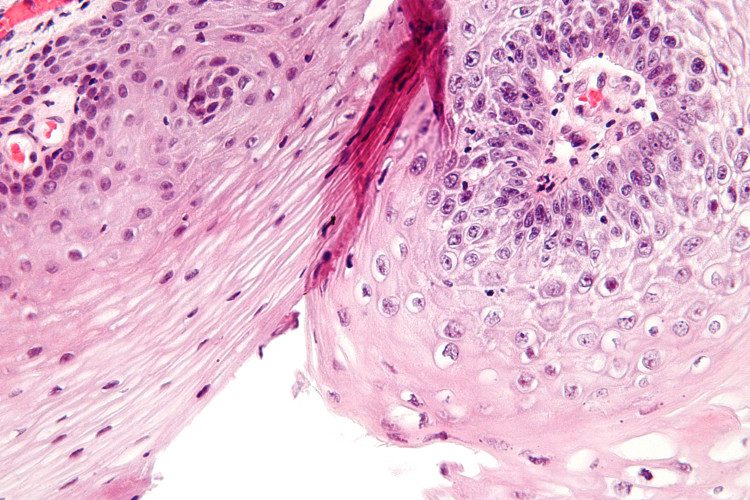
The incubation period for genital warts is typically 3 weeks to 8 months. (Image: Condyloma acuminatum).
Symptoms of Genital Warts in Men
The surface of genital warts is moist, and pressing them may cause pus to ooze out, leading to bleeding and damage. On the shaft of the penis, solitary growths appear, resembling small spikes, pink in color, with a stem or base, and are not itchy or painful. The warts can gradually increase in number and merge into larger patches with a diameter of a few centimeters, resembling either a rooster’s comb or cauliflower.
Genital warts may spread to surrounding areas such as the lower scrotum, around the anus, inside the anus, the urethra, the glans, and the groin folds. In some cases, the warts can be as large as a fist, secreting fluid and foul-smelling blood.
Symptoms of Genital Warts in Women
Due to the complex structure of the female genitalia, the disease is often harder to detect and treat. Some symptoms to recognize include:
- The first signs often appear on the labia majora, labia minora, vagina, vulva, around the anus, urethra, perineum, hymen, and cervix, with soft, bright pink or whitish bumps. They cluster together to form large areas resembling cauliflower, without causing pain or itching but are prone to bleeding.
- During sexual intercourse or other forms of contact, genital warts can easily rupture, leading to bleeding, infection, and damage at those sites. Patients may experience fatigue, loss of appetite, weight loss, painful intercourse, and decreased sexual desire.
- In addition to the typical symptoms, genital warts can also appear in the mouth during unsafe oral sex, in the eyes, and on fingers and toes. In these cases, pink bumps resembling warts cluster closely together. Oral genital warts are easily mistaken for mouth ulcers or pharyngitis, so caution is advised.
Diagnosis of Genital Warts
The lesions of genital warts are very distinctive, so diagnosis primarily relies on clinical symptoms, which involve taking a history of exposure to the source of infection and observing the characteristic lesions. Women with cervical genital warts should undergo regular pap smear tests or other examinations to detect dysplasia or cancer early.
The lesions of genital warts are very distinctive, so diagnosis primarily relies on clinical symptoms.
Treatment Methods for Genital Warts
Currently, there is no specific medication for genital warts; patients may carry the virus for life, showing symptoms or remaining asymptomatic. Treatment includes three main categories of methods, which serve only to reduce symptoms or remove lesions without eradicating the HPV virus.
- Topical medications: Small, isolated warts located externally can be treated by applying solutions such as 80-90% trichloroacetic acid, 20-25% podophyllotoxin, or 5% imiquimod directly to the lesions periodically. Avoid applying these solutions to mucous membranes, such as inside the vagina or cervix, as they can cause burns.
- Physical methods such as cryotherapy with liquid nitrogen, electrocautery, and CO2 laser can destroy warts that grow deeply.
- Surgical removal or excision of large and widespread warts is indicated for significant cases.
Prevention of Genital Warts
- The best way is to engage in sexual relationships that are faithful and monogamous.
- Avoid sexual relations with individuals whose health status is unknown. Always use condoms correctly during sexual intercourse. While condoms do not provide 100% protection, they are an effective method to reduce the risk of sexually transmitted infections.
- Maintain good personal hygiene, especially washing the genital area with soap before and after sexual activities.
- Undergo regular health check-ups to detect any diseases early.
- Seek medical attention promptly if any suspicious symptoms or signs arise.
Can STIs be transmitted in public restrooms?
Toilets are home to many types of bacteria, especially in public places that are not cleaned and sanitized, posing significant health risks.
However, most sexually transmitted infections like HIV, syphilis, and gonorrhea are transmitted through direct contact between genital organs and bodily fluids such as semen and vaginal secretions during intercourse. Only when bacteria or viruses are transferred directly from the toilet seat to the genital area or through an open wound or scrape can they cause illness. Therefore, mere skin contact in public restrooms does not typically result in these infections.
However, genital warts caused by the HPV virus are an exception. HPV is primarily transmitted through sexual contact. Nevertheless, there is substantial medical evidence that HPV can be transmitted through simple skin contact.
HPV can survive for several days on surfaces such as fingers, fingernails, or other communal contact surfaces. The virus can spread through contact, for example, via hands, feet, or toilet door handles. Thus, although rare, genital warts can be transmitted through contact when using public restrooms without handwashing, through toilet seats, or door handles…
Hand or oral sexual contact also poses a risk of transmitting HPV. In fact, hospitals have reported many cases of laryngeal and throat warts due to HPV transmission through unsafe oral sex. Notably, the HPV virus can be transmitted even when the infected person shows no signs or symptoms.
To reduce the risk of transmission, maintain good hygiene, wash your hands after using the restroom, and consider carrying hand sanitizer. When using public restrooms, you can place tissue paper on the toilet seat or wipe it with disinfectant wipes before use. While there’s no need for excessive worry, one should not be complacent. If any health concerns arise, seek medical attention promptly for definitive treatment to avoid long-term complications. (According to Master, Dr. Phan Chi Thanh, Department of Outpatient Services, Central Obstetrics Hospital).