Infections caused by antibiotic-resistant superbugs, also known as antimicrobial resistance (AMR), are emerging as a serious global health challenge. A recent global analysis report published this past Monday forecasts that in the next 25 years, nearly 40 million people could die from infections related to superbugs if timely measures are not taken to address this threat.
Superbugs – The Dangerous “Enemy” of Modern Medicine
Superbugs refer to strains of bacteria or pathogens that have developed resistance to multiple types of antibiotics, making treatment much more difficult and complex. This is one of the greatest threats to public health worldwide.
The analysis recently published in the journal The Lancet is the first study to track the global impact of superbugs over time and predict future scenarios if this issue is not controlled. According to the study, from 1990 to 2021, over a million people worldwide died each year due to AMR.
Antimicrobial resistance is an increasingly common and dangerous phenomenon.
Antimicrobial Resistance (AMR) is an increasingly common and dangerous phenomenon, where bacteria, viruses, fungi, or parasites develop resistance to the antibiotics, antivirals, antifungals, or antiparasitics used to treat infections caused by them. In other words, these medications become less effective or even ineffective against the onslaught of resistant microorganisms.
The Impact of AMR Across Age Groups
One bright spot in the report is that the mortality rate among children under 5 years old due to superbugs has decreased by over 50% in the past three decades. This improvement is believed to be due to enhanced infection prevention and control measures for infants. However, when children do contract superbugs, the infections become exceedingly hard to treat.
In contrast, the number of deaths among the elderly—especially those over 70—has increased by more than 80% during the same period. As the global population ages, they become more vulnerable to infections and face a higher risk when encountering superbugs.
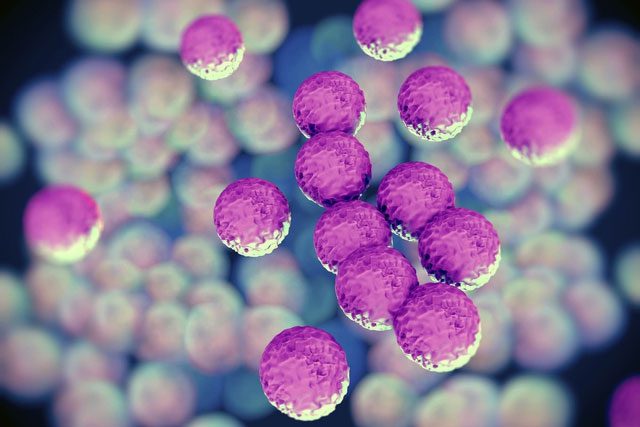
Notably, the mortality rate from MRSA (Methicillin-resistant Staphylococcus aureus), a strain of bacteria resistant to multiple antibiotics, has doubled, from 65,000 cases in the early 1990s to 130,000 cases in 2021.

When bacteria become resistant, common infections such as pneumonia, urinary tract infections, and skin infections become harder to treat, prolonging illness and increasing the risk of complications and death.
Future Forecasts: A Grim Scenario
Based on current trends, researchers predict that the direct death toll from AMR will rise by 67% in the next 25 years, estimating around 2 million deaths per year by 2050. AMR could also contribute to an additional 8.2 million deaths annually, an increase of nearly 75%, leading to a total of 169 million deaths from superbugs during this period.
The analysis indicates that AMR could directly cause 39 million deaths from now until 2050 unless strong interventions are implemented. However, a less dire scenario could occur if the global community focuses on improving healthcare for severe infections and expanding access to antibiotics. In this case, up to 92 million lives could be saved by 2050.
Treating drug-resistant infections often requires expensive specialty medications, complex treatment methods, and longer hospital stays, placing an economic burden on patients and healthcare systems.
“These findings underscore that AMR has been a significant global health threat for decades, and this threat is increasing,” said Mohsen Naghavi, a co-author of the study from the Institute for Health Metrics based in the United States. The research analyzed 22 pathogens, 84 drug and pathogen combinations, and 11 infection syndromes such as meningitis, based on data from 520 million individual records worldwide, including 204 countries and territories.
This analysis comes at a critical time, ahead of a high-level United Nations meeting on AMR scheduled for September 26, aimed at raising awareness among the international community and promoting necessary actions to prevent an impending disaster.
Many advancements in medicine, such as surgery, chemotherapy, and organ transplants, depend on the use of antibiotics to prevent and treat infections. Antimicrobial resistance could reverse these advancements and make surgical procedures more dangerous.
Why Are Drug-Resistant Superbugs Becoming Dangerous?
Antimicrobial resistance is a natural phenomenon where bacteria develop the ability to resist the antibiotics we use for treatment. However, the misuse and overuse of antibiotics in medicine, livestock, and agriculture have accelerated this process, making many types of bacteria harder to treat. As bacteria develop drug resistance, traditional treatment methods become ineffective, leading to higher mortality rates.
Not only does this impact the treatment of common illnesses such as pneumonia, wound infections, or meningitis, but superbugs also threaten advancements in modern medicine such as surgeries, cancer chemotherapy, and organ transplantation, as the risk of uncontrolled infections becomes too high.

The misuse of antibiotics makes bacteria harder to treat.
Addressing AMR requires global cooperation, including controlling antibiotic use, developing new medications, and raising awareness about the dangers of superbugs. Additionally, improving healthcare access, strengthening infection control measures, and developing effective treatment solutions are urgent measures.
In the fight against superbugs, acting now can save millions of lives and protect the future of global health from a major health crisis.