It was a moment Meagan James never expected to witness. A surgical team at NYU Langone Health in New York, USA, performed a groundbreaking transplant.
After a workplace accident that resulted in the loss of his left eye and part of his face, Aaron received a new window to the soul along with a partial face transplant.
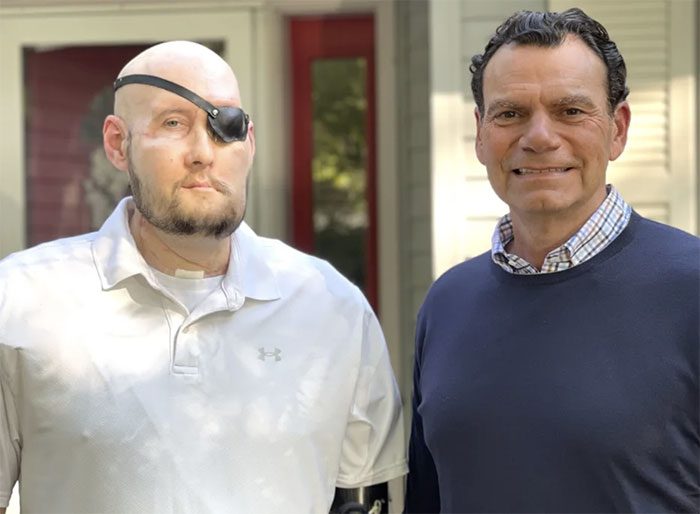
Aaron James, 46, with his surgeon, Dr. Eduardo Rodriguez, who led the full eye and partial face transplant surgery for him. (Photo: NYU Langone Health)
When Meagan first looked into her husband’s new eye, she noticed the post-surgery swelling and saw that the eye was brown. Aaron’s natural eye color was sea blue. She also saw his new nose, lips, and cheek, where a few hairs had begun to grow. She saw a face filled with gratitude, and that was when the emotions surged.
She was happy for her husband of 20 years. “It was a feeling that was crazy, wonderful, strange, overwhelming, and happy. I’m so glad he made it, and everything is good right now,” Meagan said.
At the end of May, a team of over 140 surgeons at NYU Langone Health completed Aaron’s transplant, which lasted approximately 21 hours. The surgery included a full left eye transplant and facial parts from a single donor. This was the first such transplant in medical history.
According to the medical team, Aaron’s eye is now showing “impressive” signs of health. Although he cannot yet see with his new eye, Aaron remains hopeful that over time, he will be able to see—and his first surgery may pave the way for a new field in transplant medicine.
“That’s really my biggest hope,” Aaron said. “If I can see, that would be amazing. And if it starts a new path in medical science, I’m all for it.”
The Fateful Accident
Meagan said seeing Aaron’s new eye and face “wasn’t a huge shock” compared to seeing him on the night of the accident.
Aaron, a 46-year-old veteran living in Arkansas, worked as a power line worker. One night in June 2021, while working with colleagues in Mississippi, his face accidentally touched a live power line.
The 7,200-volt electric shock caused severe trauma to Aaron’s face, destroying his left eye, entire nose, lips, left cheek, chin, and left arm.
That day in Arkansas, Meagan and their daughter, Allie, a high school student, were driving home from the grocery store when Meagan’s phone rang. The terrible, fragmented words she heard were “Aaron,” “accident,” and “serious.”
Meagan immediately packed her bags and drove about four and a half hours to Mississippi, where Aaron was receiving care at a local hospital. While driving, her phone rang again. This time it was the doctor. The doctor described Aaron’s condition and explained that he had been electrocuted.
“Is he okay? Will he be okay?” Meagan asked. She recalled the doctor’s response: “The only thing I can promise you is that he won’t die before you get here.”
Meagan remembered she often told Aaron to “be careful” every morning before he went to work. She still wonders if she reminded him to “be careful” on the morning of his accident.
“Oh God, his face is gone”
Meagan was always by Aaron’s side as he was transferred to various medical centers for more specialized care, for reconstructive surgery, and for the amputation of his left arm.
The wife recounted: “When I saw him, his jawbone was exposed. I could see his eye sockets and everything. I saw his skull. I thought, ‘Oh God, his face is gone.’ But most of my worry was about how he would be when he woke up and was aware.”

Surgeon Eduardo Rodriguez with Aaron James before the full eye and partial face transplant. (Photo: NYU Langone Health).
Aaron said he remembers nothing of the accident. “I woke up, went to work, and woke up six weeks later in Dallas, Texas. It’s a strange feeling to suddenly wake up in a hospital.”
The first time Aaron saw himself after the accident was in his hospital bed in Dallas. He asked Meagan to take a picture, but she hesitated. “Are you sure you want to take a picture?” Aaron replied: “Yeah, it will be fine.”
“She took a picture and turned the phone around, and I said, ‘Oh God, this is a bad one,’” he recalled. “I mean, I felt fine, I knew I would be okay. We just had a long way to go.”
Aaron’s medical team mentioned the option of a face transplant to Meagan.
“As soon as the face transplant was mentioned, that’s when I thought, ‘Wow, this is a big deal’ because they don’t do things like that every day,” he said.
In New York, Dr. Eduardo Rodriguez, director of the Face Transplant Program at NYU Langone Health—who had performed four previous face transplants—and his colleagues were introduced to Aaron’s case by experts in Texas. After learning more about the electrocution accident and the subsequent injuries, Rodriguez said it was impressive that Aaron had survived.
“You must have patient zero”
Discussions about the possibility of the transplant continued even after the medical team in Texas had to remove Aaron’s left eye due to severe pain. Rodriguez and his colleagues in New York requested the Texas team to preserve as many optic nerves as possible in hopes of transplanting the eye.
When Rodriguez spoke with Aaron about the possibility of performing not just a partial face transplant but also a full eye transplant, he warned that the donor’s eye might not restore vision. For vision to be possible, some communication between the transplanted eye and the brain would be necessary.
Aaron said: “But I said even if it doesn’t work, I’ll have an eye and at least it will look normal, and then all of you can learn something from this. You must have patient zero.”
Aaron was placed on the potential recipient list in February 2023. The opportunity for a full eye and partial face transplant came just a few months later, in May.
It was a “risky” procedure for Rodriguez and his colleagues. Previously, no medical team in the world had successfully performed an eye transplant on a living patient.
“It’s an entirely unexplored field,” Dr. Rodriguez said.

Dr. Eduardo Rodriguez performing the full eye and partial face transplant surgery on the patient. (Photo: NYU Langone Health)
The Stressful Surgery
The surgery involved two operating rooms. Aaron was in one room, where surgeons removed parts of his face to replace them with tissue from the donor. Rodriguez was in another room, dissecting the face and eyeball of the donor.
“That part took about 12 hours,” Dr. Rodriguez said, “At this point, I had to ensure that Aaron’s room was ready to receive the new face. We cut the blood vessels, disconnected from the donor, and the race began. At this point, the face and eye were not receiving any blood supply.”
Rodriguez and his colleagues then began connecting the donor’s face and eyeball to Aaron. To transplant the eye, the research team combined the donor’s eye with adult stem cells derived from the donor’s bone marrow by injecting the adult stem cells into the optic nerve during the transplant process. These stem cells could help enhance nerve regeneration.
“We can identify a specific cell, CD34, as an adult stem cell with potential benefits—not just in immune modulation, since this is a transplant cell—but also in nerve regeneration,” he explained further: “When connecting the optic nerve from the donor to the recipient, right at that spot, we injected those CD34 stem cells in.”
Dr. José-Alain Sahel, clinical spokesperson for the American Academy of Ophthalmology, noted that a crucial step in the full eye transplant surgery was reconnecting Aaron’s optic nerve to the donor’s eye. He wasn’t involved in this process but participated in related experimental research.
Sahel, who monitored the surgery by the NYU Langone Health team, said: “It was smart of them not to cut the optic nerve too far from the eyeball when removing the eye from the recipient.”
“I think what still needs to be done—a critical job—will be how to regenerate the optic nerve, guiding its fibers or axons to the right targets, as well as ensuring that the corneal nerves are well preserved,” Sahel said. “What we learned from this case is that surgery can be successful, and then we should push for more research, invest more in research on corneal and optic nerve regeneration.”

Dr. Eduardo Rodriguez performing a full eye and partial face transplant surgery on a patient. (Photo: NYU Langone Health).
Gratitude and Hope
Rodriguez stated that when the surgery was completed and Aaron saw his new face in the mirror for the first time, he was overjoyed. Aaron continues to be closely monitored and must take medication to reduce the risk of his body rejecting the transplant. The medical team noted that the eye showed healthy signs, such as having a direct blood flow to the retina, the layer of tissue at the back of the eyeball associated with the image processing.
Coming up, Aaron, Meagan, and their daughter Allie are preparing to celebrate Thanksgiving together. Now that Aaron can smell and taste, he is very much looking forward to the Thanksgiving meal.
He also remains hopeful that one day, he may be able to see through the eye of the donor.
Dr. Rodriguez commented: “Whether he will be able to see or not is a question that remains unanswered. But I am very hopeful.”
Dr. Oren Tepper, a plastic and reconstructive surgeon and director of the Facial Surgery Program at Montefiore Health System, stated that this procedure marks an important milestone in the field of transplant medicine.
Mr. Tepper wrote: “This complex and high-tech surgery represents a significant advancement in the field of face transplantation. Ultimately, if the eye transplant proves successful in restoring any form of neural function or visual signals, it will be a tremendous breakthrough in medicine for patients who have lost eyes due to trauma or cancer.”



















































