The importance of bones cannot be overstated. Bones keep our bodies upright, protect our internal organs, enable us to move our limbs, and support our bodies instead of collapsing on the ground. When we are young, bones grow with us and heal easily after fractures. However, as we age, bones become increasingly fragile and are often damaged, broken, or may even require surgical replacement.
The structural function of bones is already rich, but its role extends far beyond that. Our bones also store large amounts of calcium, phosphorus, and minerals, which are crucial for nerve and cellular function. Additionally, bone marrow produces hundreds of billions of blood cells each day, which are used to transport oxygen, fight infections, clot bleeding wounds, and create other cells that form cartilage and adipose tissue.
And that’s not all. In recent decades, scientists have discovered that bones also participate in complex chemical exchanges with other parts of the body, including the kidneys, brain, adipose tissue, muscles, and even the gut microbiota. It’s like suddenly realizing that the beams and wall studs in your house can communicate with the air conditioner, refrigerator, microwave… Scientists are also deciphering how bone cells send signals to other organs and how these organs interpret and respond to foreign molecular information. Clinical researchers are contemplating how to harness this cellular communication to develop new methods for protecting or strengthening bones.
This is a completely new field of exploration, and recent studies have made scientists realize that bones are much more dynamic than previously thought.
The Language of Bones – Bones Also Have “Voices”
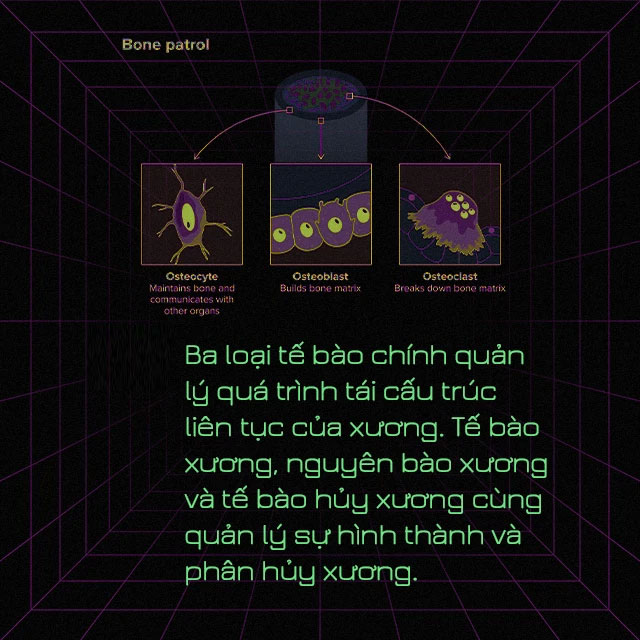
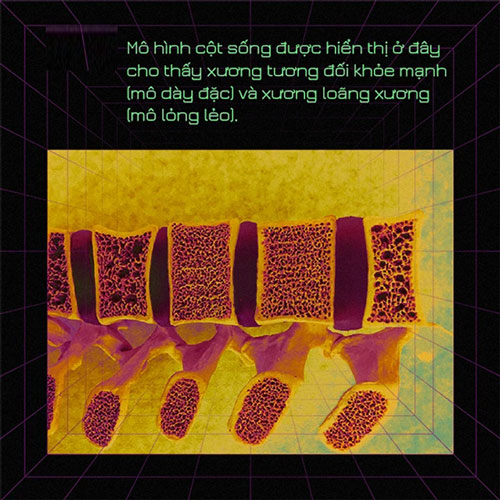
Bones are a unique “tissue” that not only contains cells that strengthen but also cells that break down, allowing bones to continue growing during childhood and regenerate broken bones throughout life. The cells responsible for building bones are called osteoblasts, while those responsible for breaking them down are known as osteoclasts. When these two types of cells operate out of balance, the body may produce too little (or too much) bone. For example, osteoporosis occurs when new bone does not form quickly enough to replace old bone that is being resorbed, making bones loose and prone to fractures.
In addition to osteoblasts and osteoclasts, bones also contain another type of cell called osteocytes. Although these cells account for over 90% of the total cells in bones, they have not been thoroughly studied. It wasn’t until 20 years ago that a cell biologist named Lynda Bonewald, working at Indiana University in Indianapolis, began to take an interest in them. Her colleagues advised her not to waste her time, as osteocytes might be nothing more than cells that sense mechanical stress and regulate bone remodeling.
But Bonewald decided to take a closer look. She and other researchers discovered that osteocytes actually sense mechanical loads. But she also pointed out, “It’s much more than that.”
She wrote studies on the importance of osteocytes for the kidneys, pancreas, and muscles, and in 2006 she published the first report on the communication of osteocytes with other organs, indicating that osteocytes produce a growth factor called FGF23.
This molecule travels through the bloodstream to the kidneys. If there is too much FGF23 in the body—such as occurs in a genetic form of rickets—the kidneys will excrete too much phosphorus in the urine, causing the body to lose this essential mineral, leading to rickets, muscle weakness, or joint stiffness and dental problems.
Around the same time Bonewald was studying osteocytes, physiologist Gerard Karsenty also began investigating the relationship between bone remodeling and energy metabolism. He hypothesized that there might be a connection between these two factors, as the process of breaking down and rebuilding bone is energy-intensive.
In a 2000 study, Karsenty analyzed the relationship between a hormone called leptin and both biological processes. Leptin is produced by fat cells and its primary role is to suppress appetite. During evolution, it appeared alongside bones. Karsenty found in experiments on mice that leptin affects the brain, halting the process of bone remodeling.
In this way, early vertebrates could suppress appetite and bone growth when food was scarce, conserving their energy for daily functions.
The research team used X-rays to scan the hands and wrists of several children who lacked fat cells (and therefore also lacked leptin) due to a gene mutation. According to the radiologist’s assessment, the bone age of these children was months, or even years, older than their actual age. This suggests that in the absence of leptin, their bones grew faster, reflecting characteristics of older bones such as higher bone density.
This was a case of bones listening to other organs, but in 2007, Karsenty proposed that bones also communicate something about how the body uses energy. He discovered that mice lacking a bone-building protein called osteocalcin had difficulty regulating their blood sugar levels.
In further research, Karsenty found that osteocalcin also promotes male fertility through its effects on sex hormone production, enhances learning and memory by altering neurotransmitter levels in the brain, and boosts muscle function during exercise. He detailed these messages and other “conversations” that bones engage in in the Annual Review of Physiology in 2012.
Whether osteocalcin plays an important role in the evolutionary process of vertebrates or not, these studies have inspired other scientists to begin investigating how bones communicate with other parts of the body.
Communication Between Muscle and Bone
In the body’s movement process, bones and muscles are a perfect “partnership,” engaging in various physical interactions. Muscles pull on bones, and as muscles grow larger and stronger, bones also become larger and stronger to counter the increased pulling force of the muscles. In this way, bones adapt to the body’s needs so that bones and muscles always work together efficiently.
However, scientists have discovered that there is also metabolic exchange between these two “partners.” For example, skeletal muscle cells produce a protein called myostatin, which prevents muscles from growing too large. Simultaneously, experiments on rodents and observations in humans show that this substance also inhibits bone mass development.
During exercise, muscles also synthesize a molecule called beta-aminoisobutyric acid (BAIBA), which affects how fat and insulin respond to increased energy expenditure. Bonewald also found that this molecule can reduce damage to bone cells from reactive oxygen species, a byproduct of cellular metabolism. In young mice that were immobilized for a long time, they would experience bone and muscle atrophy, but when supplemented with beta-aminoisobutyric acid, their bones and muscles gradually returned to normal.
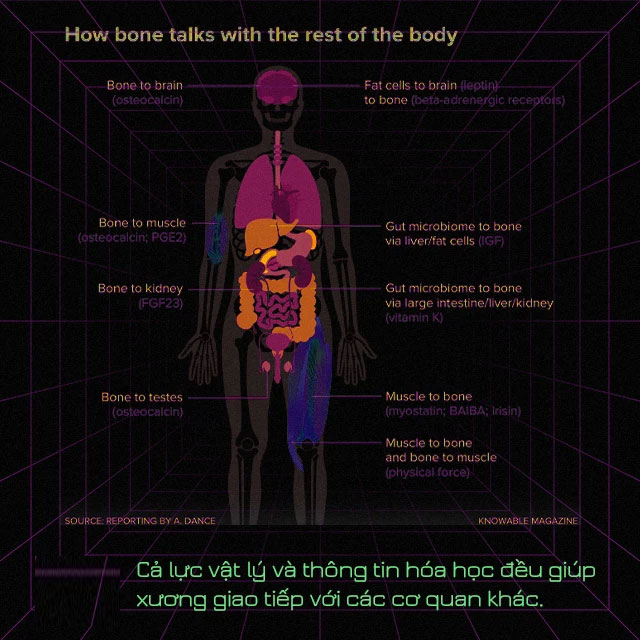
In further research, Bonewald and her colleagues also found another molecule, irisin, which increases with exercise. When cultured in vitro, this substance helps osteoclasts maintain their activity; and in animals, this molecule also promotes bone regeneration.
Moreover, this communication is not a one-time affair. In turn, osteocytes regularly produce prostaglandin E2, which helps promote muscle growth. The secretion of this molecule increases when bones sense the tension of the muscles increasing.
Communication Between Bone and Gut
Our bodies contain nearly equal numbers of cells and microorganisms. The gut microbiota acts like another organ and plays a certain role in the body. They help us digest food, prevent infections from harmful bacteria, and communicate with other organs, including bones.
So far, communication between bones and the gut microbiota seems to be one-way. No one has observed that bones transmit information to the gut microbiota, but bones can receive a lot of useful information from the gut. For example, in cases of severe food poisoning, when we need to mobilize all of the body’s resources to fight infection, this is not the best time for bone growth.
The connection between bones and the microbiome was first observed in a study conducted in 2012. The mice used in this research were raised in a sterile environment, free of any microorganisms in their bodies. They had fewer osteoclasts and, consequently, a greater bone mass. When these mice were supplemented with beneficial gut bacteria, their bone mass quickly returned to normal levels within a short period.
Health Implications
The most intriguing aspect of these findings is their potential to help us discover new methods for treating bone health, enabling medications to work effectively in various parts of the body.
It is estimated that nearly 13% of individuals over the age of 50 suffer from osteoporosis. While existing medications can slow down the bone degradation process or promote bone growth, they often come with side effects and limited effectiveness. Thus, there is a pressing need to identify new treatment approaches.
We can begin by focusing on the gut. Probiotics, along with foods containing deliberately cultivated bacteria, such as fermented dairy products, may help build a healthy gut microbiome. Lactobacillus reuteri has shown promise in helping mice combat bone loss following antibiotic treatment.
Scientists still have much to learn about the communication between bones and other parts of the body. Over time, this research may lead to more treatment options to maintain the health of bones and other bodily systems.
- Shocking encounters with a tribe of pygmies who hunt deadly snakes for food, a dish few dare to try!
- Why do hens mimicking roosters’ crowing get considered an “ominous sign” and are often killed?
- Experience on the world’s longest high-speed bridge: Drivers fear “frozen”, a pregnant woman gives birth on the bridge