Libmeldy, priced at $3.3 million per treatment, addresses rare diseases by modifying the patient’s stem cells, inserting healthy gene copies that enable the production of normal blood cells.
In February, Teddi Shaw, a 20-month-old patient diagnosed with the rare genetic disorder MLD, also known as metachromatic leukodystrophy, was successfully treated with one of the world’s most expensive drugs. The revolutionary treatment method called Libmeldy, produced by Orchard Therapeutics, is valued at approximately $3.3 million. The drug is seen as a beacon of hope for many children afflicted with MLD in the future.
Typically, children with MLD gradually lose their ability to think, move, and perceive the world around them. Eventually, they are unable to walk, swallow, speak, hear, see, or respond to bodily stimuli. Most infants diagnosed with MLD will die before they reach five years old.
MLD occurs due to one or more faulty gene segments. It is a recessive gene disorder, meaning that only children who inherit two faulty copies from both parents will develop this condition. Consequently, MLD is quite rare, affecting about one in 40,000 children in the UK. In the United States, it is estimated that fewer than 50,000 individuals have the disease.
In children with two copies of the defective gene, the level of sulfatide (a fat found in the white matter of the brain and spinal cord) accumulates excessively in the nerve cell membranes, disrupting nerve function and causing inflammation.
Doctors can treat patients with bone marrow transplants from healthy donors, but this only slows the progression of the disease. Another method is injecting active enzymes, but this is a large protein molecule that sometimes cannot cross the blood-brain barrier.
After years of research, doctors successfully tested the atidarsagene autotemcel therapy, marketed as Libmeldy. This drug provides healthy genes to create enzymes for the body.
Initially, doctors collect stem cells from the patient’s bone marrow, which can develop into various blood cell types, and send them to a laboratory in Italy. Here, scientists use a modified virus to insert healthy gene copies containing enzymes into their DNA.
Finally, the doctors inject the stem cells back into the patient’s bloodstream. The cells migrate to the bone marrow, producing blood cells that can generate enzymes and function normally.
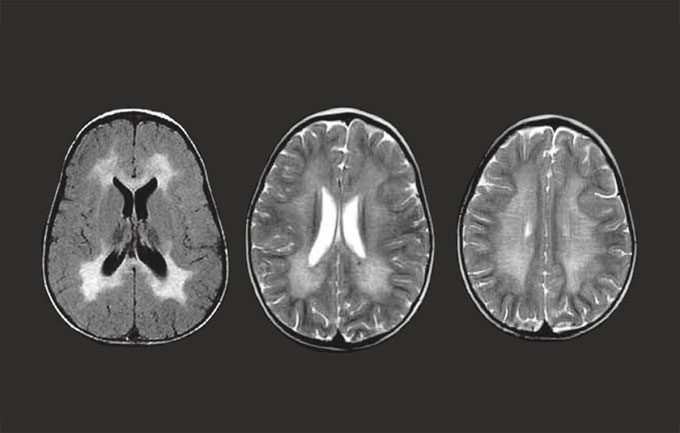
Brain of a person with metachromatic leukodystrophy. (Photo: Mldsupportuk).
In January of last year, researchers in Italy concluded that this method is effective for most children if used in the early stages of the disease. In March 2022, the National Institute for Health and Care Excellence (NICE) in the UK approved the use of the drug.
At the time of approval, Libmeldy was recognized as the most expensive drug in the world, costing £2.87 million ($3.42 million) per patient. Recently, the United States approved another gene therapy that is even more expensive, priced at $3.5 million.
Currently, Libmeldy remains the highest-priced treatment ever approved by NICE. Experts believe that this price is understandable after 20 years of research and development. Professor Bobby Gaspar, co-founder and CEO of Orchard Therapeutics, stated that bringing the drug to market has been a lengthy process involving significant effort.
A limitation of Libmeldy is that it is only effective if administered in the early stages of disease development. Many children are diagnosed with MLD only after their siblings have deteriorated. By that time, it is too late to control the life-threatening condition.
BBC reports reveal that Teddi Shaw’s older sister, three-year-old Nala, has already lost her vision and cannot walk or eat due to MLD. Nala has exceeded the age at which the drug could be used.
Researchers, doctors, and families of children with MLD are calling for screening of all newborns. However, the heel prick blood test for newborns in the UK cannot detect MLD.
The Royal Manchester Children’s Hospital is using biochemical tests to screen for the condition. This method can measure levels of sulfatide or enzyme in the patient’s blood, proving more effective than genetic testing.



















































