Since its inception, in vitro fertilization (IVF) has always been the last resort for couples struggling with infertility who want to have a baby when all other assisted reproductive solutions have failed.
What is In Vitro Fertilization?
In Vitro Fertilization (IVF) is a reproductive assistance method that involves the combination of eggs and sperm outside the body. This method is utilized after other assisted reproductive techniques have been unsuccessful and is intended for couples or women of reproductive age who, for any reason, cannot conceive naturally. Ovulation is regulated by hormones, and the fertilized egg is then transferred into the uterus.
The method is referred to as in vitro fertilization because its creator, Dr. Robert G. Edwards, conducted all his research in a standard test tube. Achieving success in 1978, this method was aptly named according to its nature at that time.
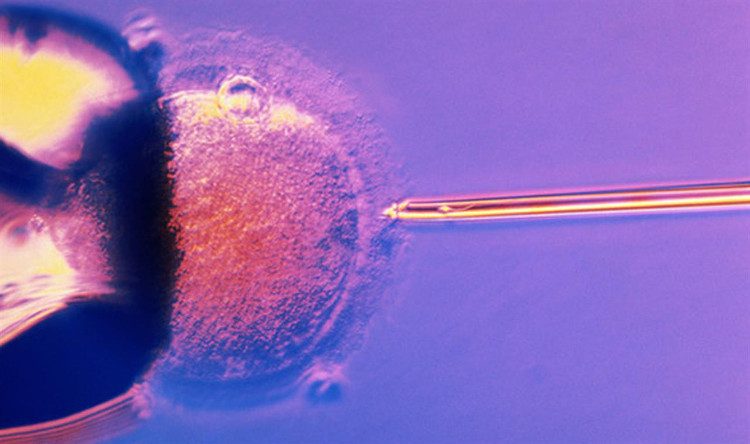
In vitro fertilization is a method of fertilization where eggs are fertilized by sperm outside the body, in a test tube.
Currently, fertilization is no longer conducted in test tubes; instead, the process occurs on Petri dishes. However, the term “in vitro fertilization” remains in use due to traditional naming conventions, as not much has fundamentally changed.
Research indicates that performing in vitro fertilization using frozen embryos has a higher success rate and offers greater safety for the embryo compared to fresh embryos taken directly from the parents’ bodies. In fact, using frozen embryos also helps reduce the risk of bleeding during pregnancy, limits premature births, and ensures adequate weight for the fetus.
In practice, in vitro fertilization is considered a lifeline for couples struggling with infertility because of its superior capabilities. Specifically, any issues related to childbirth, including problems with female reproductive organs and low sperm quality in males, can be easily addressed.
To increase the success rate of in vitro fertilization, most doctors typically implant 2-4 embryos into the mother’s body at the same time. This means that those undergoing IVF often have much higher rates of twins, triplets, or quadruplets compared to the general population. However, carrying multiple fetuses can overload the mother’s body, adversely affecting the success of the IVF process. Therefore, doctors provide the most reasonable advice for couples eager to have children.
In reality, the success rate of in vitro fertilization is not absolute. Notably, younger couples have a significantly higher success rate than older individuals attempting to conceive using this method. Specifically, the success rate for individuals under 21 is as high as 35.3%, while the success rate for those over 37 is only 27.4%. Importantly, no IVF cases have been successful for individuals over 48 years old.
The In Vitro Fertilization Process
1. Fertility Assessment Tests
Wife’s Tests
- Hormonal Testing
Hormonal testing is a quantitative test measuring the levels of various sex hormones in the blood, such as FSH, LH, estradiol, testosterone, and SHBG, to assess the hormonal status of the ovaries and related reproductive organs. This test contributes to diagnosing the remaining number of eggs in the ovaries and predicting the ovarian response to stimulation drugs in case of IVF or intrauterine insemination.
Recently, AMH (anti-Müllerian hormone) has been regarded as a more accurate hormonal test and can replace FSH, LH, and estradiol in assessing ovarian reserve. While FSH, LH, and estradiol need to be tested during the first days of the menstrual cycle (day 1 to day 5), AMH can be measured at any time during the menstrual cycle.
- Testing for Sexually Transmitted Infections
Typically, all patients seeking infertility evaluation undergo blood tests for HIV, hepatitis B, syphilis, and Chlamydia trachomatis.
Chlamydia trachomatis is a bacterium that can be transmitted sexually. For most women, Chlamydia trachomatis resolves on its own without complications. However, in some cases, the infection can ascend to the uterus and fallopian tubes, increasing the risk of infertility due to tubal damage. Therefore, screening for Chlamydia is often combined with other tests in diagnosing tubal damage.
- Gynecological Ultrasound and Follicle Count on Ovaries
Transvaginal gynecological ultrasound helps detect gynecological abnormalities such as uterine fibroids, ovarian cysts, congenital anomalies of the reproductive tract (bicornuate uterus, septate uterus, absent uterus, etc.), and polycystic ovaries.
In infertility evaluations, gynecological ultrasound should also be performed in the early days of the menstrual cycle, not only to diagnose the aforementioned abnormalities but also to count the number of follicles present on the ovaries. Follicle counting via ultrasound is a clinical factor aiding in assessing the number of remaining eggs in the ovaries and predicting the ovarian response to stimulation medications.
Husband’s Tests
- Semen Analysis
Semen analysis is a simple, cost-effective test that provides significant information for diagnosis and treatment. A semen sample is collected via masturbation after 2-7 days of abstaining from sexual intercourse. Collecting semen with less than 2 days of abstinence typically results in a lower sperm count. Conversely, excessive abstinence can reduce the percentage of motile sperm. The semen sample must be contained in a special device made from non-toxic materials for sperm.
Through the results of the semen analysis, doctors assess the quality of the examined semen sample: low sperm count, weak sperm, abnormal sperm, or no sperm at all. Except for cases of azoospermia (no sperm), semen analysis does not definitively confirm the patient’s fertility but serves as a suggestion. Sperm quality can vary between different semen analyses.
In 2010, the World Health Organization standardized and established the minimum criteria for normal semen analysis:
- Volume ≥ 1.5 ml.
- Sperm density ≥ 15 million/ml.
- Total sperm count ≥ 39 million.
- Percentage of progressively motile sperm ≥ 32%.
- Normal sperm morphology ≥ 4%.
Other Tests
The husband also undergoes screening tests for sexually transmitted infections such as hepatitis, HIV, and syphilis. In cases of azoospermia, patients may be advised to undergo additional specialized tests such as hormonal assessments (FSH, LH, Testosterone), scrotal ultrasound, and transrectal ultrasound. In some cases, a testicular biopsy may be performed before treatment decisions are made.
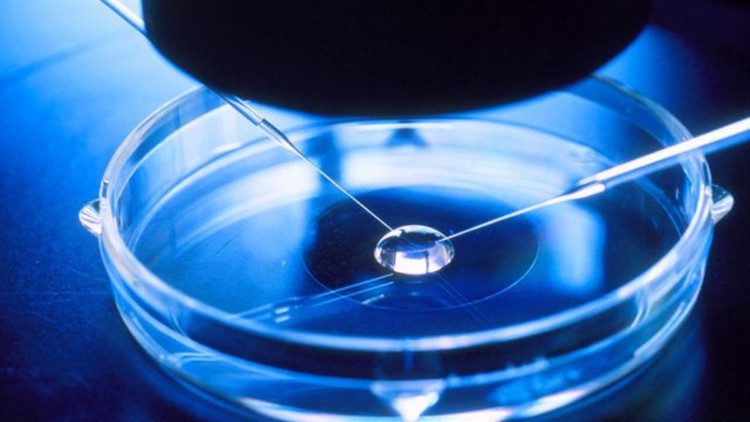
Currently, the fertilization process typically takes place on Petri dishes.
2. Pre-Anesthesia Testing
Patients undergo blood tests, urine tests, electrocardiograms, and chest X-rays to assess their health status before undergoing oocyte retrieval and pregnancy.
3. Ovarian Stimulation
Ovarian stimulation is performed based on individual cases. The duration of ovarian stimulation can vary from 2 weeks to 4 weeks, depending on whether the patient is on a short or long medication regimen.
- Follicle Ultrasound and Hormonal Measurement
The number of follicles and the development rate during stimulated cycles depend on the type of medication and stimulation protocol used. Ultrasound helps assess the number and development of follicles, allowing timely adjustment of medication dosages to achieve optimal ovarian response and minimize potential complications. During ovarian stimulation, patients will undergo follicle ultrasounds 2 to 3 times. When the follicles reach a size of 18-20 mm, patients will receive an hCG injection, a medication that helps mature the eggs and trigger ovulation.
Alongside follicle ultrasound, hormonal measurements are also essential for monitoring follicle development. Estradiol (E2) levels are commonly used to track follicle growth due to the correlation between E2 levels in the blood and follicle development. Typically, E2 levels will increase by 1.5 to 2 times the previous day’s level, indicating good follicle development.
Additionally, measuring LH and progesterone levels will help predict egg quality. Generally, the levels of these two substances in the blood are low during ovarian stimulation. If LH and progesterone levels rise excessively, it may degrade egg quality and embryo quality.
4. Oocyte Retrieval
The patient will undergo oocyte retrieval approximately 36-40 hours after hCG injection. The procedure is performed via the vaginal route, and the patient will receive local anesthesia and general anesthesia. The patient should not eat or drink anything for 4 hours prior to the egg retrieval. After retrieval, the oocytes are transferred to the laboratory for processing and combined with the husband’s sperm to form embryos. Once the eggs and sperm are combined to create embryos, they will be cultured in vitro for 2 to 3 days or 5 days before being transferred into the wife’s uterus.
5. Embryo Transfer
Embryos that have been cultured in vitro for 2-3 days (or 5 days) will be transferred into the wife’s uterus. The number of embryos transferred depends on the wife’s age, the cause of infertility, the number of previous cycles, and the current quality of the embryos. The doctor will determine the number of embryos transferred to achieve the highest pregnancy rate while minimizing the risk of multiple pregnancies.
Typically, an average of 2-3 embryos are transferred, with a pregnancy success rate of about 35-40%. After the embryo transfer, the patient only needs to rest for 1-2 hours in the clinic before being able to resume normal activities. If there are any viable surplus embryos, the patient will be advised on freezing them for potential use in future cycles. The patient will take medication to support embryo implantation for 2 weeks before pregnancy testing.
6. Pregnancy Test
This is performed 2 weeks after the embryo transfer. The patient will have their beta-hCG levels measured in the blood. If the pregnancy test result is positive, the patient will be scheduled for an ultrasound to confirm the pregnancy 3 weeks later. Higher beta-hCG levels increase the likelihood of multiple pregnancies.
7. Pregnancy Ultrasound
The ultrasound is performed 3 weeks later if the beta-hCG result is positive. The purpose of the ultrasound is to accurately determine the presence of pregnancy, the number of embryos, and their condition.
Dos and Don’ts During In Vitro Fertilization
- Diet
The patient can eat normally and does not need to avoid any foods during the ovarian stimulation and after embryo transfer. Patients at risk of ovarian hyperstimulation should consume high-protein foods (meat, fish) and drink plenty of water to help reduce the risk of hyperstimulation.
- Lifestyle
The husband should refrain from smoking as it can affect sperm quality, thereby impacting embryo quality and pregnancy outcomes. The wife should avoid heavy lifting and refrain from intense physical activities during ovarian stimulation and after embryo transfer. Sexual intercourse should also be avoided during ovarian stimulation and after embryo transfer.



















































