One of these advancements has helped terminal cancer patients, previously considered untreatable, achieve complete remission.
Medical Innovations Inspired by Science Fiction
Throughout history, medicine has been a tool to alleviate pain and extend life. The modern medical achievements we enjoy today are sometimes the result of research conducted centuries ago, such as the advent of X-rays, insulin, painkillers, and antibiotics.
However, there are also ultra-modern treatment methods that scientists are currently researching and testing. Compared to a century ago, these tools may seem like science fiction. Yet, they are poised to become a reality serving humanity in the coming years.
1. Advanced Surgical Robots: Semi-Automatic and Fully Automatic
Currently, doctors are using various types of medical robots, including those for pelvic surgery, spinal surgery, eye surgery, and intrathecal injections—all of which require extreme precision.
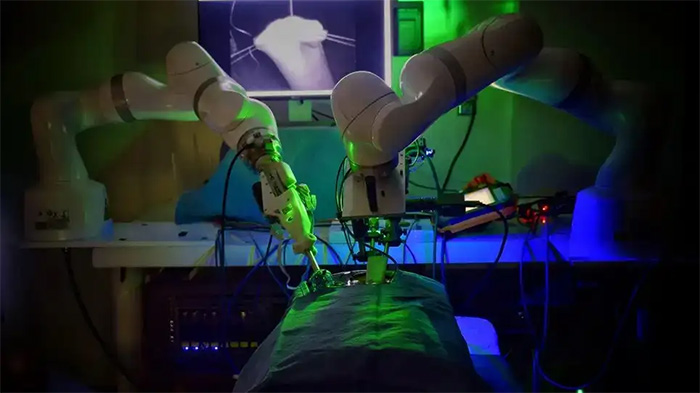
Current surgical robots are only semi-automatic.
However, current surgical robots are only semi-automatic. This means they are designed like machines, operated by technicians and doctors.
Surgeons who wish to operate these machines must complete a certification course, similar to obtaining a driver’s license. But just like cars equipped with self-driving features, surgical robots are also being developed to operate autonomously.
Earlier this year, Johns Hopkins University in the United States successfully performed the first complex soft tissue surgery using a machine called STAR. STAR is an intelligently programmed robot that successfully sutured two segments of intestine together. This is one of the most sophisticated procedures in abdominal surgery and operates entirely autonomously.
Johns Hopkins considers this a milestone, “a significant advance toward fully autonomous surgery on humans.” In the near future, robots like STAR will not only assist human doctors but may also operate independently in emergency situations, such as treating trauma patients en route to the hospital.
2. Brain Implants for Treating Depression
This method is known as deep brain stimulation. It involves implanting a pulse generator and electrodes inside the skull to provide signals that can alter or regulate abnormal activity occurring in the brain.
Previously, deep brain stimulation was commonly used to treat epilepsy and Parkinson’s disease. It is estimated that over 260,000 Parkinson’s patients worldwide have had pulse-generating devices implanted in their brains. These patients arrived at the hospital with severe tremors, but after undergoing deep brain stimulation, their conditions improved or even resolved completely.
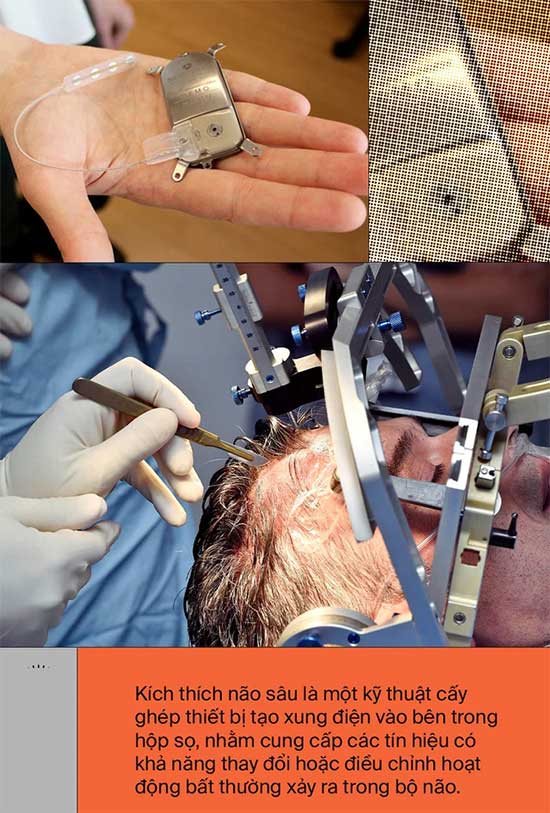
For decades, scientists have tried to use deep brain stimulation to treat depression. This work also involves implanting a pulse-generating device in the brain, a battery-operated machine the size of a matchbox that emits regular electrical signals to areas of the brain responsible for processing emotions.
The basic idea of the scientists is that if they can stimulate certain brain regions associated with depression, such as Brodmann area 25, a brain area rich in serotonin transporters that is highly active when we feel sad, patients will be able to escape their depressive episodes.
Last year, a research team at the University of California successfully tested a deep brain stimulation device on a patient with severe depression. This was a woman in her 30s named Sarah who did not respond to any of the 20 prescribed medications and therapies for depression.
It was only after receiving the deep brain stimulation implant that her condition began to improve. On the depression scale, her score dropped from 33, indicating very severe depression, to 14, and finally below 10.
Sarah has now become the first and only patient to successfully treat depression through deep brain stimulation surgery. “The device has helped me stop my depression, allowing me to become the best version of myself and rebuild a life worth living,” she said.
3. Drug-Releasing Contact Lenses
Sometimes, a medical innovation does not come from developing new and better drugs, but from finding better ways to deliver them to patients. We know that medications can be administered orally, via injection, inhalation, and even rectally.

In the future, drugs may be delivered through the eyes.
Now, there is another entry point into the body that doctors want to explore, which is the eyes.
Currently, there are two methods to deliver medication into a patient’s eye. For mild conditions like cataracts and glaucoma, medications can be applied directly to the outer surface of the eye for absorption. However, the downside of eye drops is that they can be diluted by tears.
As much as 95% of the active ingredient from eye drops may not have a chance to penetrate because tears will wash them away. Additionally, many patients report that they often forget to administer their medication on time.
The second method of delivering medication to the eye is through direct injection with a syringe. This method is commonly applied for conditions affecting the deeper areas of the eye, such as diabetic retinopathy and macular degeneration.
However, it is clear that no doctor would want to inject a patient’s eye due to the risk of infection, bleeding, and the pain it would cause the patient.
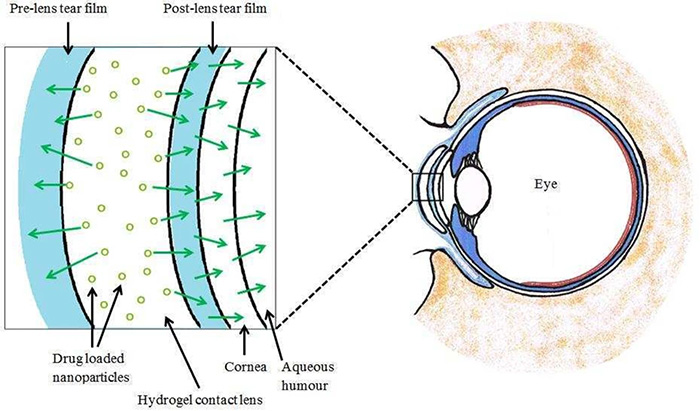
This type of contact lens allows certain shaped drug molecules to pass through.
The latest solution, a slow-release drug-releasing contact lens recently approved by the U.S. Food and Drug Administration (FDA), will address all the weaknesses of the two previous methods.
Developed by researchers at Johnson & Johnson, this contact lens features soft polymer contact points that allow certain shaped drug molecules to pass through.
It is currently approved by the FDA for the delivery of allergy medications, but in the near future, this contact lens will also be used to deliver antibiotics, anti-inflammatory drugs, and other treatments for eye conditions such as glaucoma, infections, and cataracts.
4. Gene Therapy for Cancer and Genetic Disorders
For decades, scientists have hoped to develop gene editing methods to treat difficult or seemingly incurable diseases. Now, their efforts are beginning to pay off.
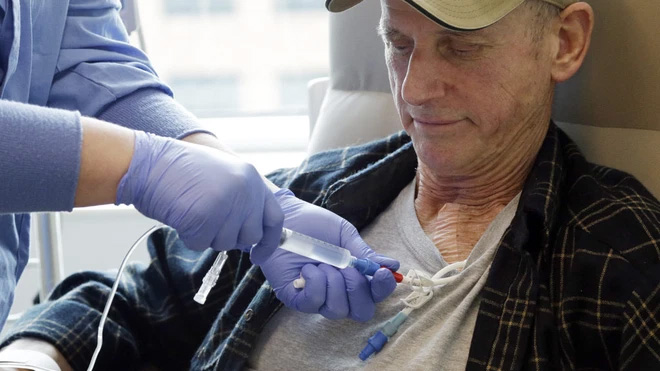
This new gene therapy aims to correct or replace harmful mutations directly causing diseases.
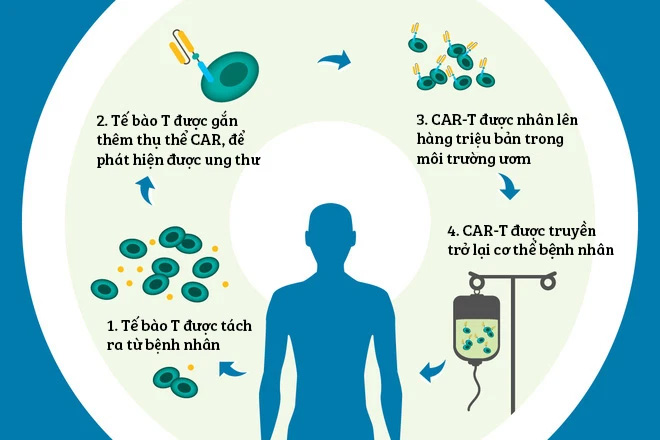
In 2017, the FDA approved at least two gene-targeted therapies aimed at correcting or replacing harmful mutations directly causing diseases. One method called CAR-T involves editing a person’s T cells in the laboratory to help them fight cancer.
Specifically, doctors extract T cells from the patient’s immune system and find ways to combine them with chimeric antigen receptors (CAR). After forming the CAR-T combination, this drug is infused back into the patient’s body.
The CAR receptor will seek out and attach itself to target cancer cells. As a result, T cells can attack the cancer, which they were unable to do before when they viewed the cancer cells as a normal part of the body.
In several clinical trials and real case studies, CAR-T has shown remarkable effectiveness. It has helped some terminal cancer patients, previously considered untreatable, achieve complete remission.
The second therapy showing promise is gene editing for sickle cell disease. Sickle cell disease is a dangerous congenital genetic disorder affecting millions of people worldwide. Typically, red blood cells are round, flexible, and move easily through blood vessels.
However, children born with a gene mutation that produces abnormal hemoglobin have red blood cells that become rigid, sticky, and crescent-shaped. These abnormally shaped cells often get stuck in small blood vessels, leading to slowed or blocked blood flow, which carries oxygen and nutrients to various parts of the body.
Currently, there is no cure for sickle cell disease, aside from pain management and preventive treatments for related complications.
However, in a clinical trial result published last December, scientists reported successfully repairing sickle cells using a gene editing technique.
A type of medication was injected directly into the bone marrow area containing blood-forming cells, helping to correct genetic defects and produce normal, healthy red blood cells for patients over three years.
With these successes, scientists indicate that the application of gene therapy will soon be expanded to other genetic diseases and various types of cancer.
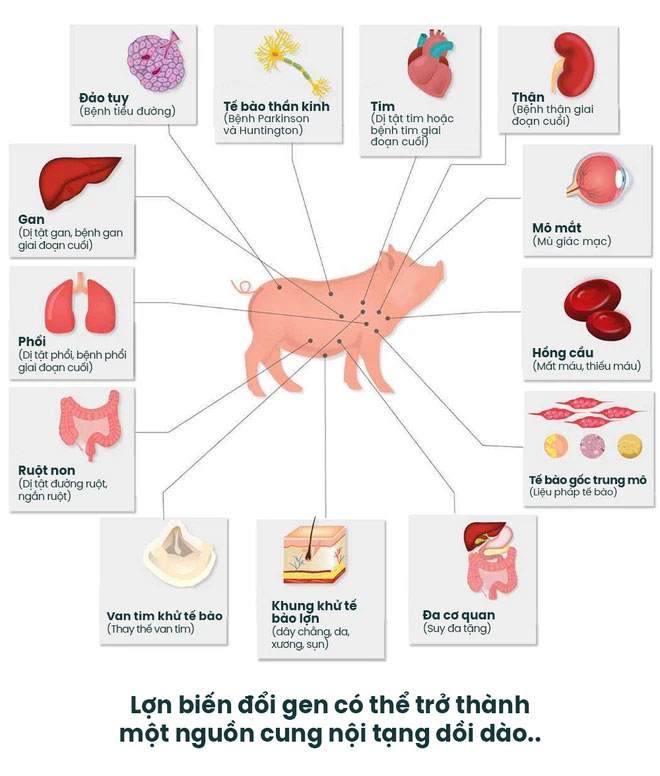
5. Pig Organ Transplants into Humans
For centuries, doctors have dreamed of transplanting animal organs into humans. This could address the shortage of organ supplies and save millions of patients each year. This concept, known as xenotransplantation, has been tested since 1667 but has yet to achieve official success.
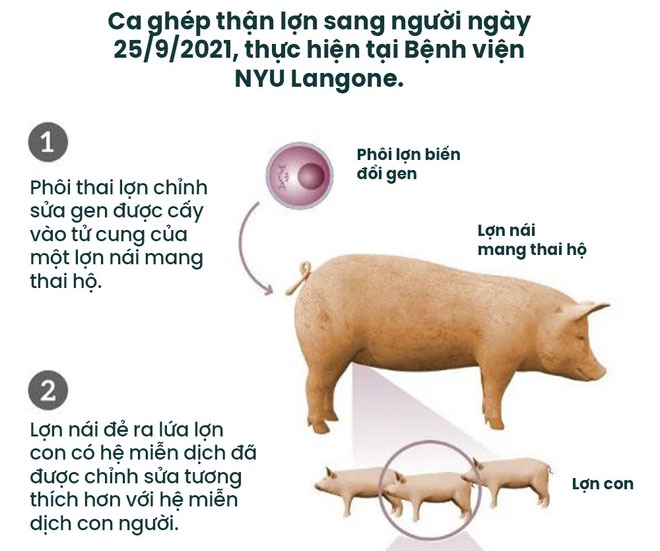
The years 2021 and 2022 marked significant milestones with two successful transplants of pig kidneys and hearts into humans, yielding promising results.
In September of last year, a doctor at New York University named Robert Montgomery successfully transplanted a pig kidney into a patient with kidney failure and brain death. Although the procedure did not officially save the patient, Dr. Montgomery stated that the transplant confirmed the pig kidney functioned normally in the human body without being rejected.
For 54 hours, the pig kidney produced urine and brought the patient’s creatinine levels back to normal—a sign that the pig kidney had alleviated the patient’s kidney failure.
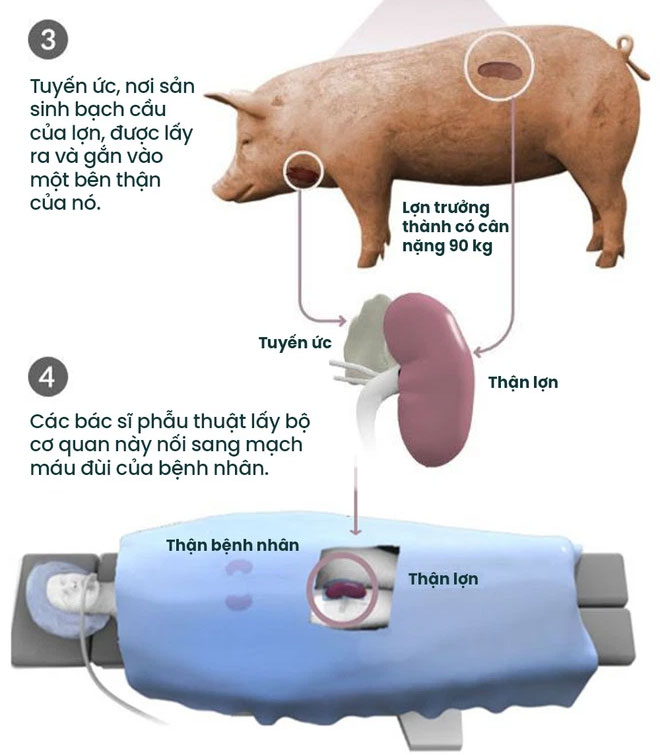
By January of this year, a team of doctors at the University of Maryland Medical Center successfully transplanted the first pig heart into a patient with severe heart failure, allowing him to live for an additional two months.
Although not perfect, these initial experiments have shown that pig organs can survive the transplant process without being immediately rejected by our immune system.
“Like any first transplant surgery performed in the world, this surgery has led to valuable insights, providing hope and lessons for doctors to improve outcomes and save patients in the future,” said Dr. Bartley P. Griffith, who performed the pig-to-human heart transplant.


















































