In 1901, Karl Landsteiner discovered that the serum of one person could agglutinate the red blood cells of another, and vice versa. Subsequently, the A and B antigens, antibody A (against A), and antibody B (against B) were identified. To date, many antigens have been discovered. Based on the presence of these antigens on the surface of red blood cells, blood groups are classified into systems such as ABO, Rh, Duffy, Kidd, Lewis, Kell, P, and MNSs. Among these, the ABO and Rh blood group systems are particularly significant due to their critical role in blood transfusions.
Each blood group has its unique characteristics, and the structure of blood vessels can be compromised if an incompatible blood type is transfused. Therefore, knowing your blood type and its properties is very important.
Why are there different blood types?
Scientists believe that the adaptation of human ancestors to infectious diseases is the reason for the emergence of different blood types. For example, malaria is thought to be a major factor in the prevalence of blood type O, which is more common in Africa and regions of the world that have been burdened by malaria. In many cases, malaria-infected cells cannot invade the cells of blood type O or blood type B. As a result, individuals with blood type O tend to have better resistance to malaria.
How are blood types classified?
Human blood is categorized into various groups based on specific carbohydrates and proteins found on red blood cells. There are about 46 different blood groups, but the main ones are O, A, B, and the Rh factor. Each blood group can have antibodies against the others. Therefore, when blood from a different group is transfused, the recipient’s antibodies may destroy the transfused blood, causing harm to the body.
Antigens and antibodies
In general, an antigen is “any substance that can provoke an immune response”. The membrane of each red blood cell contains millions of antigens that the immune system ignores, although it will attack any red blood cells that contain antigens different from its own.
Antibodies are important molecules that our immune system produces to help protect the body against invading agents such as bacteria and viruses. These bacteria and viruses can also form in response to different blood groups.
There are about 46 different blood groups, but the main ones are O, A, B, and the Rh factor.
Rh Factor
Most people (about 85% of the population) possess a special protein on their blood cells known as the Rh factor. These cases are referred to as Rh+ (Rh positive blood type). Individuals lacking the Rh factor are termed Rh- (Rh negative blood type).
Pregnant women need Rh factor testing in their blood to screen and detect compatibility between the mother and the baby. If the mother is Rh- and the baby is Rh+, the mother’s body will react to the baby’s blood as if it were a foreign substance. The mother will produce antibodies against the Rh+ blood of the baby. Rh incompatibility can cause complications in subsequent pregnancies, as the Rh antibodies can cross the placenta and attack the baby’s red blood cells, leading to hemolytic anemia in the baby, meaning the red blood cells are destroyed.
Fortunately, if Rh incompatibility is detected early, doctors can implement prenatal treatments to prevent any issues before they arise.
What are the blood types?
Blood Type A
Blood type A is characterized by the presence of A antigens on red blood cells and B antibodies in the plasma.
Individuals with blood type A can safely donate blood to others with the same blood type A or to those with blood type AB. Additionally, people with blood type A can also receive blood from individuals with blood type O.
Blood Type B
This blood type is relatively rare (only second to AB). It contains B antigens on red blood cells and A antibodies (to attack A antigens) in the plasma.
Individuals with blood type B can safely donate blood to others with the same blood type B or to those with blood type AB. Moreover, people with blood type B can also safely receive blood from individuals with blood type O.

Blood type O is the most common blood type.
Blood Type AB
This blood type is uncommon. Blood type AB is characterized by having both A and B antigens on red blood cells, and no antibodies in the plasma.
Individuals with blood type AB can accept blood from anyone. However, due to the presence of both antigens on AB red blood cells, people with blood type AB can only donate blood to others with the same blood type AB.
Blood Type O
Blood type O is the most common blood type. Blood type O has neither A nor B antigens on red blood cells, but it has both A and B antibodies in the plasma. As a result, individuals with blood type O can only receive blood from others with blood type O, as the antibodies in their plasma will attack other types. However, those with blood type O can donate blood to all other blood types, as blood type O has no hostile antigens in the immune system. Thus, individuals with blood type O are referred to as “universal donors.”
What happens if you receive the wrong blood type?
It’s very serious. Acute hemolytic transfusion reactions can occur within 24 hours after a blood transfusion and often happen during the transfusion process. Patients may experience reactions such as a burning sensation at the transfusion site, chills, fever, and pain in the back or flanks. These reactions can lead to severe hemolysis; the red blood cells from the transfused blood are destroyed by the recipient’s antibodies while still in the bloodstream. Systemic reactions can cause shock, and the large amount of tissue generated due to the rupture of red blood cells (RBCs) can uncontrollably affect clotting ability.
Principles of Blood Transfusion
To ensure safety in blood transfusions, the following principles must be adhered to:
- Blood must be transfused from the same group to avoid the corresponding antigens and antibodies from reacting, causing agglutination of red blood cells.
- In addition to determining the blood type of the donor and recipient, cross-matching must be performed: mix the donor’s red blood cells with the recipient’s serum and vice versa. If there is no agglutination of red blood cells, then the blood can be transfused to the recipient.
- If blood is incompatible, it can lead to serious complications for the blood recipient, potentially resulting in death within a few days.
However, in emergency situations requiring a blood transfusion without compatible blood available, the following minimum principle must be observed: “Donor red blood cells must not agglutinate with recipient serum.” Only a small amount of blood (250ml) should be transfused at a very slow rate. Thus, the blood transfusion diagram may look like this:
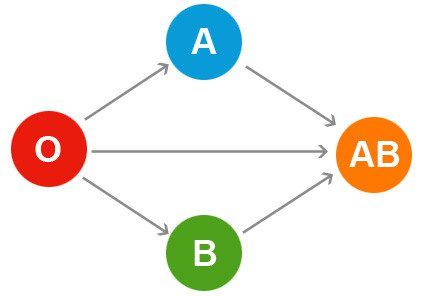
Blood transfusion diagram.


















































