When the SARS-CoV-2 virus invades, the body activates a complex response system, with antibodies being just one component of the entire human defense system.
Since the outbreak of the Covid-19 pandemic, the types of antibodies that help humans combat the SARS-CoV-2 virus have been the focus of attention and are considered a protective shield against the disease.
However, the reality is that the response against SARS-CoV-2 in the human body is “a complex and synchronized machinery”, involving many parts and cellular systems, according to scientist Roger Shapiro, an immunologist at Harvard University, as reported by AFP.
The Human Body’s Defense Mechanism
In recent weeks, public interest in antibodies has intensified, as some studies show that Covid-19 vaccines do not produce as many antibodies to prevent the Omicron variant compared to older variants like Alpha or Delta.
Antibodies are produced by the body through two pathways: either through vaccination with various vaccines or through natural infection.
The SARS-CoV-2 virus enters the human body via a spike protein on the virus’s surface. This is the part that antibodies focus on attacking, thereby neutralizing the virus’s ability to invade host cells.
However, antibodies are not the only factors contributing to the complex immune response of humans.
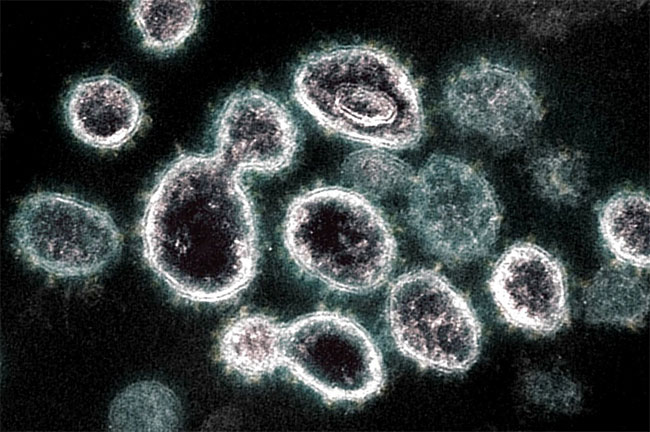
SARS-CoV-2 Virus. (Photo: AFP).
When the virus begins to invade the human body, within a few minutes to a few hours, warning proteins send out alarm signals that activate the natural immune system, mobilizing white blood cells to combat the pathogen.
The first line of defense cells produced at the site of infection are neutrophils, which make up 50-70% of the body’s white blood cells. However, neutrophils have low combat effectiveness and disappear quickly.
Other types of white blood cells then join the process of eliminating foreign pathogens, such as macrophages and eosinophils.
“The body mobilizes a large number of white blood cells to the area where the pathogen invades to eliminate the foreign pathogen as much as possible,” said John Wherry, an immunology expert at the University of Pennsylvania.
The white blood cell-based response mechanism is the body’s first line of defense, aimed at extending the time for other parts of the immune system to produce effective response cells against the pathogen, according to Professor Wherry.
The Final Line of Defense
If the foreign pathogen is not eliminated in the initial “carpet bombing” of white blood cells, the immune system’s “adaptive” response will begin to operate.
Within a few days after the body becomes infected, B lymphocyte recognition cells detect the pathogen and begin to produce antibodies.
For vaccinated individuals, the vaccine previously administered plays a training role for B cells—primarily located in lymph nodes near the injection site—preparing them to react when facing the actual pathogen.
The most effective type of antibody is the “neutralizing antibody.” This type of antibody functions like chewing gum sticking to the “keys,” which are the spike proteins of the virus, preventing the virus from unlocking and entering cells.
Other types of antibodies with lower binding capabilities slow the virus’s progress or pull the virus towards immune cells, enhancing the overall defensive response.

Simulation of antibodies attacking the virus. (Photo: Brunel University).
The partner of B lymphocytes is the T lymphocyte. T lymphocytes are divided into two types: helper and killer.
“Killer T cells will attack infected cells,” explained Professor Roger Shapiro of Harvard University.
Throughout the process of destroying infected cells, T cells may also cause unwanted damage to the body.
Meanwhile, helper T cells coordinate the activities of immune cells while stimulating B lymphocytes to produce more antibodies.
Due to significant mutations in the spike protein, the Omicron variant likely carries the ability to evade neutralizing antibodies generated through vaccination or natural infection. This means the risk of humans contracting the Omicron variant is higher than with previous virus strains.
However, T cells are not easily evaded by new variants like antibodies. According to Professor Wherry, during the virus’s replication process inside the human body, T cells can recognize the components of the virus.
T cells can detect characteristic signs of viruses they have encountered before, even when the virus has mutated.
Killer T cells are responsible for finding and destroying infected cells. They puncture infected cells, triggering responses to produce inflammatory proteins called cytokines to eliminate the virus.
Depending on the speed of the immune response, individuals who have received the full vaccine doses are likely to experience only mild symptoms, like a cold, or moderate symptoms, like the flu. The risk of severe illness in this group has been shown to be very low.
For those who have received a booster vaccine, the production process of all types of antibodies is stimulated. The booster shot also further enhances the activity of B and T cells.
“Omicron is a concerning variant, but it will not be able to completely evade the immune system’s response,” said Professor Wherry.


















































