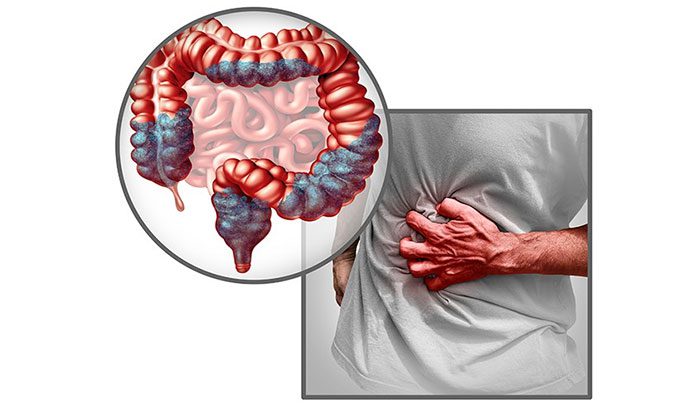
Irritable Bowel Syndrome is a common gastrointestinal disorder characterized by recurrent abdominal cramps, along with discomfort for the patient.
Irritable Bowel Syndrome: Causes, Symptoms, and Treatment
Most cases of Irritable Bowel Syndrome (IBS) have no clear direct cause. IBS is common, costly, and affects the quality of life of patients, thus it is important to understand and manage it well to improve life quality.
Understanding Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is one of the most common bowel disorders, with a prevalence rate of 5-20% in the population. This syndrome is benign; although it is not life-threatening, it significantly impacts the quality of life of those affected. IBS is more commonly diagnosed in women, with a female-to-male ratio of about 1.25-2/1, and is typically diagnosed in individuals aged 20 to 50 years. It is characterized by recurring abdominal pain, changes in bowel habits, and feelings of bloating and discomfort in the abdomen. It is a functional bowel disorder that recurs multiple times without any identifiable structural lesions during examinations.
IBS is classified into four types based on the symptoms experienced by the patient. The treatment methods may vary accordingly:
- IBS with constipation
- IBS with diarrhea
- Mixed IBS (experiencing both diarrhea and constipation)
- IBS unspecified
While no specific studies have identified the direct causes of IBS, food has been shown to be a contributing factor that stimulates the digestive system, leading to contractions, abdominal pain, and discomfort. Additionally, medical studies indicate a correlation between IBS symptoms and food. Therefore, the quality and safety of food can significantly influence the condition.
Symptoms of Irritable Bowel Syndrome
The hallmark symptom of IBS is recurrent abdominal pain. This pain is often related to bowel movements, changes in bowel habits, and the nature of the stool. Clinical signs affect the daily activities of the patient, causing inconvenience in lifestyle, eating, and health deterioration.
Patients should note that these symptoms may recur at irregular intervals and can be exacerbated by prolonged stress or the consumption of low-quality foods that may cause allergic reactions.
The hallmark symptom of Irritable Bowel Syndrome is recurrent abdominal pain.
1. Abdominal Pain
Abdominal pain: The pain does not have specific characteristics, lacks a definite location, is experienced along the colon, and is often heightened after eating or sometimes even before finishing a meal. Pain often occurs in the morning and may ease after a bowel movement. The pain may be vague, intermittent, or cramp-like, due to bowel dysfunction and increased bowel motility. This pain recurs at least once a week and has persisted for the past three months.
2. Constipation or Diarrhea
IBS is classified based on the stool characteristics as either constipation or diarrhea. Constipation is defined as having fewer than three bowel movements per week, with stool varying from hard lumps to soft, watery forms. It is important to note that there should never be blood in the stool; if blood is present, it may indicate underlying gastrointestinal diseases.
3. Other Signs
Other clinical signs of IBS include:
- Bloating and flatulence
- Cramps
- Fatigue
- Muscle aches
- Sleep disturbances
- Feeling of incomplete bowel evacuation
- Excessive gas
4. Alarm Signs
The following signs are considered alarm signs and should not be ignored; screening for underlying gastrointestinal diseases is necessary:
- Onset of symptoms after the age of 50
- Presence of blood in the stool
- Unintentional weight loss
- Palpable abdominal or rectal masses
- Nocturnal symptoms (pain or diarrhea)
- Anemia
- Fever
- Abdominal distension
- Family history of colorectal cancer or chronic inflammatory bowel disease
Causes of Irritable Bowel Syndrome
The causes of IBS have not been clearly identified. However, experts indicate that emotional factors, dietary habits, and medication can directly influence the symptoms of gastrointestinal diseases.
IBS can be described as a condition resulting from a combination of physiological and psychosocial factors. These triggers can also stimulate the recurrence or worsening of the condition.
1. Stress
Stress is a common cause of gastrointestinal-related diseases, including IBS. When a person is stressed, the central nervous system affects gastric and intestinal functions through the autonomic nervous system. Therefore, stress is considered a factor that increases the risk of developing IBS.
2. Hormonal Factors
Hormonal imbalances are a cause of IBS related to abnormal hormone changes. Hormones are part of psychosocial factors that predispose individuals to develop IBS. Hormonal factors are a collection of glands that produce hormones in the body, responsible for balancing metabolism and maintaining reproductive and sexual functions.
Hormonal imbalances can lead to abnormal hormonal changes, resulting in gastrointestinal dysfunction and increased likelihood of altered bowel motility, leading to IBS.
3. Food
Food is considered a primary cause of IBS. Spoiled or unsuitable foods for the individual can stimulate the stomach and colon. These stimuli can increase bowel motility, causing IBS.
4. Family History of the Disease
A family history of gastrointestinal disorders is also a factor that increases the sensitivity of the bowel, making one more susceptible to IBS than others.
This factor is not a direct cause of IBS, but if you have a family member with a history of IBS, it is essential to be proactive in maintaining your digestive health.
Irritable Bowel Syndrome can occur in any individual, regardless of age. However, it is more common among those aged 20 to 50 years. Furthermore, women are twice as likely to develop IBS compared to men.
Factors that may increase your risk of developing IBS include:
- Frequent stress and anxiety
- Having mental health issues such as depression or anxiety disorders
- A history of or currently suffering from severe gastrointestinal infections
- Irregular and unscientific eating habits or skipping meals
- Having a family member who has experienced IBS
Diagnosis of Irritable Bowel Syndrome
IBS is primarily diagnosed through the clinical symptoms presented by each patient. During the clinical diagnosis process, the doctor will require the patient to provide information about their health and family history. Based on this information, the doctor will proceed to order appropriate additional tests. In practice, IBS diagnosis is clinical, based on symptoms and exclusion of underlying gastrointestinal diseases, with patients not exhibiting any of the aforementioned alarm signs, accompanied by normal test results.
1. Gastrointestinal Endoscopy
Gastrointestinal endoscopy is the main tool for diagnosing gastrointestinal disorders. Esophagogastroduodenoscopy and colonoscopy will be performed based on the current symptoms and medical history of the patient. A biopsy will be conducted if the doctor identifies any suspected or confirmed lesions during the endoscopy.
2. Testing
Testing is a clinical diagnostic method used to identify the causes of Irritable Bowel Syndrome (IBS).
There are several types of tests related to the diagnosis of IBS, including:
- Blood tests to rule out disorders caused by sensitivity to proteins and to exclude other systemic diseases.
- Stool tests if the patient experiences diarrhea, aimed at checking for bacteria or parasites in the stool, as well as calprotectin tests in normal cases to consider IBS.
- Lactose intolerance testing.
Treatment for Irritable Bowel Syndrome
The treatment for Irritable Bowel Syndrome focuses primarily on diet and nutrition, along with medication to address prominent symptoms and adopting a scientific lifestyle to restore and improve colon function.
IBS treatment protocols are tailored to the specific symptoms experienced by each patient. Therefore, doctors will prescribe medications based on the symptoms and guide patients on dietary regimens, necessary supplements, and foods to avoid due to potential allergies.
Common medications used in the treatment of IBS include:
- Antispasmodic medications
- Medications for diarrhea
- Medications for constipation
- Fiber supplements
- Calming medications for anxiety
- Probiotics
Additionally, patients need to follow a suitable diet, increasing fiber intake from fruits and vegetables. They should also minimize foods high in gluten such as wheat, oats, and cereals. For those who test positive for allergies to proteins in these foods, complete elimination from their diet is necessary.
IBS patients are encouraged to follow a low FODMAP diet to stabilize the colon and improve digestive health. This diet restricts foods that are short-chain carbohydrates, such as apples, watermelon, canned fruits in general, lactose-containing milk, cheese, yogurt, fructose and high-fructose fruits, honey, legumes, beets, broccoli, wheat, and alcoholic beverages.
Is Irritable Bowel Syndrome Dangerous?
Irritable Bowel Syndrome is not a dangerous condition. IBS cases are usually diagnosed at a mild level, with patients experiencing recurring abdominal pain and bowel irregularities, and serious physical impacts are very rare.
In some mild cases, the condition may resolve on its own without medication, simply requiring dietary adjustments. Therefore, if you suspect you have IBS or have been diagnosed, you should not stress or worry, as this may exacerbate your symptoms.
However, patients should not be complacent and must take treatment seriously to prevent worsening or prolonging symptoms, which could affect other organs in the digestive system. Patients should also seek medical examination and advice to rule out serious gastrointestinal disorders before being assured that it is IBS – a benign condition.
Preventing Irritable Bowel Syndrome
The best way to prevent Irritable Bowel Syndrome is to protect digestive health and avoid all related digestive disorders. The exact causes of IBS have yet to be identified, so maintaining a stable digestive system is crucial to reducing the risk of developing related conditions, including IBS.
The most important proactive measure to prevent Irritable Bowel Syndrome and other digestive disorders is through diet and lifestyle habits. Here are some tips to improve the nutritional quality of your meals:
- Minimize skipping meals or eating irregularly
- Eat slowly, avoiding fast consumption
- Limit consumption of spicy, greasy, and canned or processed foods
- Reduce alcohol and carbonated beverages
- Control intake of high-fructose fruits, not exceeding 240g per day
Irritable Bowel Syndrome is a common digestive disorder characterized by disturbances in the digestive tract, marked by recurrent abdominal pain and changes in bowel habits, leading to various inconveniences in daily life. The main treatment method focuses on symptom management combined with a diet tailored to each individual’s needs.


















































