Cirrhosis is considered one of the “four incurable diseases”. Particularly with the habits of consuming alcohol and beer, the high rate of hepatitis virus infection, and the current issue of contaminated food, cirrhosis is becoming increasingly common. To understand more about what cirrhosis is, its symptoms, and its effects, let’s explore the article below.
What is Cirrhosis?
Cirrhosis occurs as a response to liver damage. Whenever the liver is injured, it will attempt to repair itself, with healthy liver cells being replaced by fibrous tissue, scarring, and the formation of nodules. As more and more scar tissue accumulates, liver function declines, and the liver can no longer perform its normal activities.
The liver performs several essential functions, including detoxifying harmful substances in the body, cleansing the blood, and producing vital nutrients. Although the liver works quite hard, it often “manages on its own” when sick; when the liver is damaged, the remaining healthy tissue can still cope with daily metabolic activities, not immediately signaling that the liver is impaired. Therefore, it is not easy to detect liver disease. Significant symptoms only appear when liver damage exceeds 70%.
About 80–90% of patients with liver cancer have previously gone through the initial stages of chronic hepatitis, cirrhosis, and then liver cancer. Therefore, the progression of liver cancer is often summarized in “three steps”: Hepatitis – Cirrhosis – Liver Cancer. Decompensated cirrhosis is a term used to describe the development of specific complications caused by changes associated with cirrhosis, which can threaten life.
Liver damage due to cirrhosis is often irreversible, but if cirrhosis is diagnosed early and the underlying cause is addressed, it may be possible to limit further liver damage.

Comparison image of a healthy liver and a diseased liver.
Symptoms of Cirrhosis
As mentioned above, it is very difficult to detect liver diseases early; thus, in the initial stages, the symptoms of cirrhosis are quite vague. However, as more scar tissue replaces healthy tissue and liver function declines, you may experience the following symptoms:
Early Stage Cirrhosis
Early-stage cirrhosis, often referred to as compensated cirrhosis, is the period when a patient transitions from chronic hepatitis to cirrhosis. In this stage, due to good compensatory ability, the healthy parts of the liver “shoulder” additional work of the damaged liver sections, and patients show few signs of liver function decline. Therefore, symptoms of cirrhosis during this stage are usually minimal, and patients may present with:
- Discomfort inside, indigestion, bloating, dyspepsia, digestive disorders.
- Fatigue, possibly with a mild fever in the afternoon.
- Intermittent pain in the right upper abdomen, gradually increasing over time.
- Dark yellow urine.
- Enlarged liver and spleen.
- Appearance of spider veins on the back, chest, hands, and legs.
- Thinning armpit and groin hair.
- Dry, white fingernails, with men experiencing testicular atrophy and breast shrinkage. In women, decreased libido may lead to amenorrhea, while in men, decreased libido can lead to erectile dysfunction.
- The compensated cirrhosis stage can remain stable for many years but often progresses gradually with episodes. The disease can rapidly worsen under favorable conditions.
End-Stage Cirrhosis
The decompensated cirrhosis stage, often referred to as end-stage cirrhosis, is the stage at which the liver is severely weakened and nearly loses its ability to function. This stage is also called decompensated because the liver cells can no longer compensate for those that have become fibrotic. At this point, 80% to 90% of the liver structure has been destroyed by fibrous tissue and is beyond recovery. Patients will exhibit the following symptoms:
- Significant health deterioration, severe digestive disorders, and black stools.
- Swelling in one or both legs, soft to the touch, with a dent remaining for 1 to 2 minutes after pressing.
- Abdominal swelling due to ascites. If there is too much fluid, it can compress arteries, causing esophageal varices to rupture, leading to massive bleeding and potential death.
- Jaundice may appear, initially with light yellow skin, which then progresses to a deeper yellow, with the yellow color spreading from the palms to the rest of the body.
- Patients may experience confusion, alternating between being semi-conscious and unconscious due to the liver’s inability to filter ammonia, leading to brain toxicity.
- Endocrine function is also affected; males may experience typical cirrhosis symptoms such as testicular atrophy, breast enlargement, and decreased libido, while females often experience menstrual irregularities or amenorrhea.
- Patients may have mental disturbances such as loss of concentration and sleep disorders. If the disease progresses severely, patients may become agitated, restless, and gradually slip into a coma, potentially leading to death.
At this stage, liver function has severely declined. Supportive treatment primarily focuses on alleviating pain for the patient and managing symptoms with pain relievers, diuretics, and treatments for edema.
High-Risk Groups for Cirrhosis
Cirrhosis is a disease that is difficult to detect in its early stages, with typical symptoms only appearing when the disease is severe, making treatment for cirrhosis more challenging than ever. Those at high risk for cirrhosis should be aware and proactive in getting check-ups for early detection of the disease. These include:
- Individuals with or having liver issues such as fatty liver, alcohol-related hepatitis, viral hepatitis, or liver inflammation.
- Alcoholics or those whose jobs require frequent alcohol consumption.
- Overweight or obese individuals, or those who regularly consume high-fat foods.
Causes of Cirrhosis
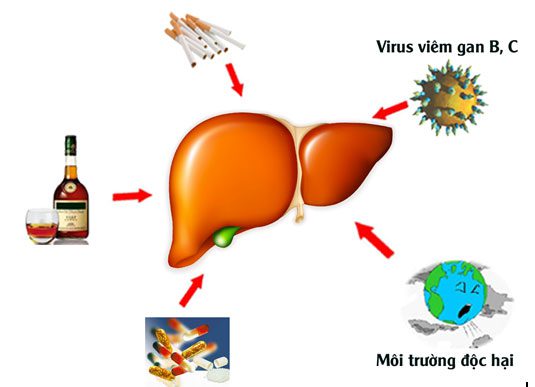
Causes of cirrhosis.
Currently, several main causes have been identified as culprits of cirrhosis:
- Alcoholic Beverages: Alcoholic drinks, including beer and spirits, are often the primary causes of liver problems, especially when consuming impure homemade spirits that contain harmful toxins that can severely damage liver cells. Prolonged excessive drinking can lead to fatty liver disease, which may then progress to cirrhosis. Research indicates that consuming about 40-60ml of alcohol per day increases the risk of cirrhosis by six times compared to non-drinkers; for those drinking around 60-80ml daily, the risk increases to fourteen times. Nearly 60% of individuals with chronic alcoholism develop fatty liver disease, and 20%-30% will progress to cirrhosis.
- Viral Infections: Hepatitis B and C, when left untreated or improperly managed over time, can significantly contribute to the development of cirrhosis. Research data show that 15%-20% of patients with hepatitis will develop cirrhosis within six years, with 10%-15% of cirrhosis patients progressing to liver cancer. Among patients with cirrhosis and liver cancer, 80%-90% are at risk of carrying the hepatitis B virus. If untreated, approximately 90% of these patients will die from cirrhosis or liver cancer within 30 to 50 years.
- Parasitic Infections: Poor dietary habits and inadequate food safety controls increase the risk of parasitic infections. Many people unknowingly consume parasites through undercooked food. For instance, liver flukes can stimulate fibrous tissue proliferation in the liver, potentially leading to increased venous pressure and cirrhosis due to these parasites.
- Biliary Cirrhosis: Bile buildup due to inflammation, obstruction, or gallstones can negatively affect the liver and its cells, potentially leading to cirrhosis.
- Obesity: Obesity is a major cause of non-alcoholic fatty liver disease, which occurs when excess fat accumulates in liver cells. While the exact cause of this condition is not fully understood, it is often associated with metabolic disorders, high blood pressure, and elevated triglycerides, which commonly occur with obesity. Excess fat in the liver can also lead to cirrhosis and liver failure. Although individuals aged 40-50 are generally at higher risk, obese adolescents are also susceptible to this condition.
- Sugary Drinks: High-sugar soft drinks can contribute to obesity, which in turn affects liver health. A study found that individuals who consume at least one sugary drink daily are more likely to develop fatty liver disease than those who do not consume any. The risk is even greater for those who are already overweight or obese.
- Acetaminophen-containing Medications: High doses of acetaminophen can lead to liver failure or even death. It is advisable not to exceed the recommended dosage of medications containing acetaminophen and to limit oneself to a single product containing this ingredient, as it is present in many over-the-counter medications, including cold remedies.
- Genetic Disorders: Certain genetic conditions can lead to liver disease, such as hemochromatosis, which causes iron accumulation in the body, resulting in cirrhosis and liver failure. Additionally, Wilson’s disease can harm not only the liver but also the brain and other organs. Fortunately, these conditions can be treated.
- Autoimmune Diseases: When the body’s immune system mistakenly attacks the liver, it can lead to autoimmune hepatitis. The cause of this condition is unclear but may have genetic roots. It typically affects women, especially those with other autoimmune disorders. Primary biliary cholangitis is another autoimmune disease that impacts women and can lead to cirrhosis and liver failure if untreated.
- Smoking: Smoking increases the risk of liver cancer and cirrhosis. The toxic chemicals in cigarette smoke can cause inflammation, cirrhosis, and increase the production of cytokines, which worsen liver cell damage. Those with hepatitis B and C who smoke are at a higher risk of developing hepatocellular carcinoma.
- Gastrointestinal Bleeding: In advanced cirrhosis, blood flow through the liver is obstructed, leading to increased pressure in the portal vein and the systemic venous system. Additionally, gastric and esophageal veins may become weakened. If these veins become excessively dilated, they can rupture, resulting in vomiting blood or passing black stools. In such cases, patients must be taken to emergency care immediately to prevent life-threatening situations.
Treatment for Cirrhosis
Modern medicine currently lacks specific medications to reverse fibrotic liver cells. The primary goal of treating cirrhosis is to reduce complications and limit the progression of damaged liver cells.
Treatment for cirrhosis typically depends on the underlying cause, so patients need to identify the cause of their cirrhosis to mitigate and prevent these factors from worsening their condition. In the early stages of cirrhosis, minimizing liver damage is the top priority.
- Treatment for Alcohol-related Cirrhosis: Patients with cirrhosis due to excessive drinking should stop consuming alcohol. If quitting drinking proves difficult, doctors may recommend an alcohol cessation program.
- Weight Loss: For patients with cirrhosis not caused by alcohol, but rather by fatty liver disease, improving their condition may be possible through weight loss and better blood sugar control.
- Medications for Liver Disease: Certain medications can help prevent liver cell damage caused by hepatitis B and C.
- Medications for Cirrhosis Symptoms: Some medications can slow the progression of cirrhosis.
Cirrhosis often leads to complications, some of which include:
- Fluid retention: A low-sodium diet and medications can prevent fluid buildup in the body to manage edema. Paracentesis may be required for severe cases.
- Increased portal vein pressure.
- Infection: Antibiotics may be administered for patients with infections.
- Risk of developing liver cancer.
- Hepatic encephalopathy.
Additionally, patients need to rest adequately, avoid strenuous activity and overexertion, and take medications as prescribed by their doctors. If significant ascites occurs, hospitalization may be necessary for daily treatment and monitoring of blood electrolytes.
Cirrhosis patients should establish a balanced diet and lifestyle, limiting high-fat and high-cholesterol foods, increasing fiber intake, and ensuring adequate nutrition. Engaging in regular exercise, avoiding late nights, and maintaining a relaxed mindset are also crucial.
To prevent this dangerous condition of cirrhosis, we should:
- Implement effective measures to prevent hepatitis virus infections.
- Limit the consumption of alcoholic beverages.
- Ensure a nutritious diet.
- Prevent liver fluke infections.
- Provide comprehensive treatment for bile duct diseases.
- Follow prescribed medications.
- Undergo regular liver check-ups.


















































