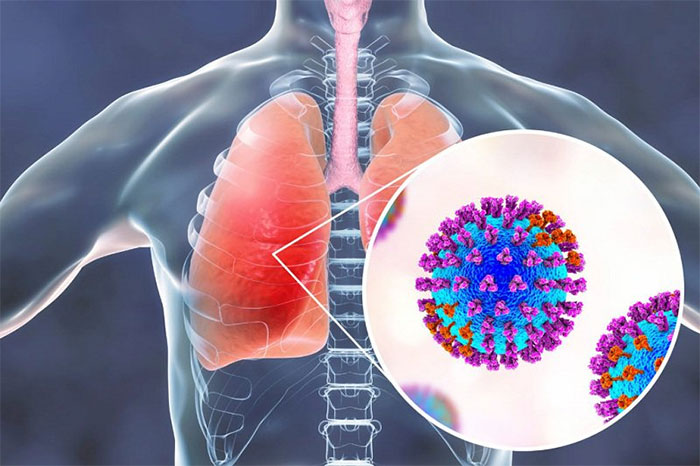
Pneumonia is an inflammatory condition of the lung parenchyma, including inflammation of the alveoli, alveolar sacs, bronchioles, interstitial connective tissue, and terminal bronchioles. The alveoli and airways in the lungs can become filled with fluid or pus, leading to symptoms such as productive cough, fever, chills, and shortness of breath.
Essential Information About Pneumonia
- Symptoms of Pneumonia
- Causes of Pneumonia
- At-Risk Groups for Pneumonia
- Diagnosis of Pneumonia
- Serious Complications of Pneumonia
- Treatment for Pneumonia
- Prevention of Pneumonia
- Caring for Pneumonia Patients
- Common Questions About Pneumonia
- 1. Can a blood test determine if someone has pneumonia?
- 2. Can a newborn’s cough indicate pneumonia?
- 3. Is bronchiolitis the same as pneumonia?
- 4. Does pneumonia require hospitalization?
- 5. Are there dietary restrictions with pneumonia?
- 6. Is antibiotic treatment necessary for pneumonia?
- 7. Can pneumonia resolve on its own?
- 8. Is pneumonia dangerous?
- 9. Is pneumonia curable?
- 10. How does pneumonia differ from lung cancer?
- 11. Does pneumonia recur?
- 12. Can pneumonia cause diarrhea or back pain?
Typically, there are many factors that can cause pneumonia, but it is most often due to bacteria, viruses, and fungi. Pneumonia can range in severity from mild inflammation to severe pneumonia. It is particularly dangerous for infants, young children, and individuals over 65 with underlying health conditions or weakened immune systems.
Pneumonia can be classified in various ways depending on the cause and the purpose of classification. Generally, pneumonia is classified based on the cause of the inflammation and the source of infection.
Classification of Pneumonia by Cause
- Bacterial Pneumonia
- Viral Pneumonia
- Fungal Pneumonia
- Chemical Pneumonia
Classification of Pneumonia by Source of Infection
- Hospital-Acquired Pneumonia
- Community-Acquired Pneumonia
Symptoms of Pneumonia
The manifestations of pneumonia can vary from mild to severe, depending on factors such as the type of pathogen causing the pneumonia, the patient’s age, and overall health. Mild signs and symptoms often resemble those of a cold or flu but tend to last longer.
Pneumonia can range in severity from mild inflammation to severe pneumonia.
Signs and symptoms of pneumonia may include:
- Chest pain when breathing or coughing
- Persistent cough, possibly producing phlegm
- Fatigue
- Fever, sweating, and chills
- In elderly or immunocompromised individuals, fever may be absent
- Nausea, vomiting, or diarrhea
- Shortness of breath
- Elderly individuals may experience confusion
Pneumonia in infants and young children may not present with any warning signs. However, children may show signs such as:
- Vomiting
- High fever, seizures
- Coughing
- Restlessness, fatigue
- Difficulty breathing, refusal to eat or drink
- Cyanosis, lethargy, retraction of the chest wall
Causes of Pneumonia
Bacterial Pneumonia
Bacteria are the leading cause of most cases of community-acquired pneumonia in adults. Bacterial pneumonia is often transmitted through respiratory droplets (when a healthy person inhales droplets containing bacteria after an infected person coughs or sneezes). Individuals with weakened immune systems or chronic underlying conditions are more susceptible to bacterial pneumonia than healthy individuals.
Viral Pneumonia
Currently, the most dangerous viral pneumonia is caused by the SARS-CoV-2 virus. Additionally, pneumonia can be caused by various other viruses that lead to colds and flu.
Fungal Pneumonia
This type of pneumonia occurs from inhaling fungal spores and is common in individuals with chronic health issues or weakened immune systems. Fungal pneumonia develops rapidly, as the spores attach to the lungs when inhaled. Smokers and those living in dusty, damp environments are at a higher risk of fungal pneumonia.
Chemical Pneumonia
Chemical pneumonia, also known as aspiration pneumonia, is a rare but highly dangerous condition. The severity of chemical pneumonia varies depending on the type of chemical, duration of exposure, the patient’s health status, and any first aid measures taken. Furthermore, chemicals that cause pneumonia may also harm other organs.
Hospital-Acquired Pneumonia
This occurs after 48 hours of hospitalization when the patient did not previously show symptoms of pneumonia. Hospital-acquired pneumonia is often caused by bacteria such as Pseudomonas aeruginosa, Acinetobacter spp., Enterobacteriaceae, Haemophilus spp., Staphylococcus aureus, and Streptococcus spp.
Community-Acquired Pneumonia
Community-acquired pneumonia refers to all types of pneumonia that are not hospital-acquired. The causes of community-acquired pneumonia are diverse, but the most common are bacterial and viral infections.
At-Risk Groups for Pneumonia
Children
Children under 5 years old, especially those under 2 months, are at the highest risk for developing and dying from pneumonia. According to the World Health Organization (WHO), approximately 150 million episodes of pneumonia occur in children in developing countries each year, with about 11 million requiring hospitalization. Pneumonia is one of the leading causes of death in children under 5 years old. The organization estimates that around 4,300 children die from pneumonia globally each day. In Vietnam alone, about 2.9 million children are diagnosed with pneumonia annually, resulting in approximately 4,000 deaths.
Pregnant Women
During pregnancy, women’s immune systems are weakened, making them more susceptible to viral and bacterial infections. Therefore, pregnant women are at a higher risk of developing pneumonia. Pneumonia during pregnancy can severely impact the health of both the mother and the fetus, increasing the risk of complications, preterm birth, and miscarriage. Notably, while a healthy individual with mild pneumonia may be treated at home and recover within 2 to 3 weeks, pregnant women who suspect they have pneumonia should seek immediate medical attention and treatment as directed by their healthcare provider to avoid affecting the fetus.
Elderly Individuals
Elderly individuals often have weakened health and poor adaptability, making them vulnerable to respiratory illnesses, including pneumonia, especially during transitional weather. If pneumonia in the elderly is not treated promptly, it can lead to serious complications, particularly respiratory failure.
Other Risk Factors
Patients in hospitals are at a higher risk of pneumonia, especially if they are in intensive care units or using ventilators.
Individuals with chronic conditions such as asthma, chronic obstructive pulmonary disease (COPD), or heart disease are more likely to develop pneumonia.
Smoking damages the body’s natural defense system against bacteria and viruses that cause pneumonia.
Individuals with weakened or suppressed immune systems, such as those infected with HIV/AIDS, organ transplant recipients, or those undergoing chemotherapy or long-term steroid treatment, are at increased risk of pneumonia.
Methods for Diagnosing Pneumonia
Pneumonia can present with clear clinical symptoms, but there are many cases where pneumonia is asymptomatic. Doctors will rely on the patient’s condition and order laboratory tests to diagnose and identify the underlying cause of pneumonia.
Clinical Examination
The doctor will take a medical history to look for signs of cough, shortness of breath, fever, and other accompanying symptoms. They will also check for dangerous signs such as difficulty breathing, cyanosis, and lethargy.
Respiratory rate will be monitored to assess whether the patient is breathing rapidly or slowly.
Lung auscultation will be performed to detect abnormal sounds such as crackles or wheezes.
Laboratory Tests
- Blood Tests: These tests check for signs of lung infection through white blood cell counts.
- Sputum Culture: This test looks for bacteria or fungi causing lung infections, allowing doctors to identify the best antibiotics for treatment.
- Chest X-ray: Chest X-rays help diagnose pneumonia. They can reveal images of lung tissue damage, such as alveolar damage and interstitial lung disease.
- CT Scan: This method is particularly important for accurately diagnosing lung opacities, revealing even the smallest or hardest-to-detect lesions that X-rays might miss.
- Bronchoscopy: This procedure allows doctors to observe the airways using a flexible tube (bronchoscope) to diagnose lung conditions. It also enables tissue, cell, or fluid samples to be collected from the lungs.
The combination of clinical and laboratory assessments helps doctors differentiate pneumonia from other serious conditions such as airway obstruction, asthma, congenital lung diseases, or other causes of respiratory failure, including cardiovascular diseases (heart failure, congenital heart disease).

Pneumonia can have clear clinical symptoms, but there are many cases where pneumonia is asymptomatic.
Dangerous Complications of Pneumonia
Even with treatment, some people with pneumonia, especially those in high-risk groups, may experience complications, including:
Sepsis
Bacteria can enter the bloodstream from the lungs, potentially infecting other organs and causing organ failure.
Respiratory Failure
If pneumonia is severe or you have chronic lung diseases, you may experience difficulty breathing and require supplemental oxygen. Hospitalization and the use of a ventilator may be necessary until the lungs heal.
Pleural Effusion
Pneumonia can cause fluid to accumulate in the thin space between the layers of tissue lining the lungs and the chest cavity (pleura). If the fluid accumulation increases and causes difficulty breathing, you may need to undergo drainage or aspiration of the fluid.
Lung Abscess
An abscess occurs if pus forms in a cavity within the lungs. Abscesses are typically treated with antibiotics. Sometimes, surgery or drainage through a needle or long tube placed into the abscess is necessary to remove the pus.
Treatment Methods for Pneumonia
Treatment for pneumonia involves addressing the infection and preventing complications. People with community-acquired pneumonia can often be treated at home with medication. However, Dr. Nguyen Thi Mong Trinh, a respiratory specialist at Tam Anh General Hospital, states: “All cases of pneumonia in children under 2 months are considered severe and must be hospitalized for treatment.”
Home Treatment
Most symptoms improve within a few days or weeks, but fatigue may last for a month or more. When treated at home, your doctor will prescribe medication based on the cause of pneumonia. You will also be scheduled for follow-up visits or advised to go to the hospital immediately if you experience complications such as difficulty breathing or high fever that does not subside.
Hospital Treatment
Adults with severe pneumonia exhibiting signs of labored breathing need to be taken to the hospital for timely treatment. For infants under 2 months old showing signs of pneumonia, immediate emergency hospitalization is required. Children aged 2-5 who are not eating, experiencing seizures, lethargy, or wheezing should also be hospitalized immediately.
Medications for Pneumonia Patients
The medications for treating pneumonia depend on the type and severity of pneumonia, as well as the patient’s age and overall health. Doctors typically prescribe:
Antibiotics: These medications are used to treat bacterial pneumonia. It may take time to identify the bacteria causing pneumonia and select the best antibiotic for treatment. If symptoms do not improve, the doctor may suggest a different antibiotic.
Antipyretics/Pain Relievers: Patients may take these medications as needed to reduce fever. These include drugs such as aspirin, ibuprofen (Advil, Motrin IB, and others), and acetaminophen (Tylenol, and others).
Preventing Pneumonia
Vaccination
Vaccines are now available to prevent certain types of pneumonia and influenza. Notably, the pneumococcal vaccine for children is widely used. Doctors recommend vaccinating against pneumonia for children under 2 years old and those aged 2 to 5 who are at special risk for pneumococcal disease. The PCV 10 vaccine, marketed as Synflorix, helps protect against 10 different strains of pneumococcal bacteria. For adults, several COVID-19 vaccines are available, including AstraZeneca, Pfizer-BioNTech, Moderna, and Johnson & Johnson’s Janssen.
Enhanced Hygiene
To protect yourself from respiratory infections that can sometimes lead to pneumonia, wash your hands frequently or use hand sanitizer, and wear masks. You should gargle daily with salt water or antiseptic solutions. This habit helps kill bacteria in the throat, thin mucus, clear airways, and minimize complications from infections.
Avoid Active or Passive Smoking
Cigarette smoke can damage the lungs’ natural ability to protect against respiratory infections.
Maintain a Strong Immune System
Ways to boost your immune system include getting enough sleep, exercising regularly, and eating a healthy diet.
Caring for Pneumonia Patients
Rest
Children with pneumonia symptoms should not attend school, and individuals with viral pneumonia also need to rest and limit interactions until recovery.
Stay Hydrated
Drink plenty of fluids, especially water, to help thin mucus in the lungs, making it easier to cough up.
Follow Prescribed Medications
Take medications exactly as prescribed. Stopping medication too early when symptoms improve can leave bacteria in the lungs to multiply, leading to a relapse of pneumonia.
Ensure a Clean Living Environment
Pneumonia is a highly contagious disease, so it is essential to maintain hygiene and prevent transmission by regularly changing the bedding, sheets, and blankets for the patient. In cases of caring for elderly patients with acute pneumonia who are comatose and bedridden, using antibacterial diapers can help ensure better personal hygiene.
Common Questions About Pneumonia
1. Can blood tests indicate pneumonia?
Blood tests can help determine the presence of infection through white blood cell counts. Doctors may take blood from a vein for culture to identify the bacteria causing illness in cases of pneumonia with septic complications. However, sputum tests are typically used to identify the specific bacteria causing pneumonia.
2. Does a cough in infants mean pneumonia?
The most common symptoms in infants with pneumonia are cough and productive cough with wet mucus or phlegm. However, the initial signs of pneumonia in infants are often subtle and unclear, such as poor feeding or refusal to feed, fever above 37.5 degrees Celsius or hypothermia, rapid breathing over 60 times per minute, or difficulty breathing.
3. Is bronchiolitis the same as pneumonia?
Bronchiolitis and pneumonia share some similar symptoms that can be confusing. However, bronchiolitis causes inflammation in the small branching tubes in the lungs, while pneumonia is an infection within the lungs.
4. Does pneumonia require hospitalization?
Not all cases of pneumonia in children require hospital treatment. Children can be treated at home if the condition is mild to avoid further infection from bacteria or viruses in the hospital, known as hospital-acquired infections.
5. Are there dietary restrictions for pneumonia?
Many studies indicate that a diet high in salt, meat, and refined carbohydrates can increase mucus production and coughing. Those who consume more meat, refined carbohydrates, and sodium are at a higher risk for persistent cough compared to those who eat more beans and fruits. Therefore, when dealing with pneumonia, it is advisable to limit red meat, processed foods, and refined grains.
6. Do You Need Antibiotics for Pneumonia?
Typically, acute pneumonia caused by bacteria, viruses, fungi, or parasites is treated with antibiotics for a duration of 7 to 14 days. In cases of severe pneumonia characterized by symptoms like shortness of breath and retraction of the chest, antibiotic treatment may extend to 15 to 20 days.
7. Can Pneumonia Resolve on Its Own?
Statistics show that there are over 50 types of pneumonia ranging from mild to severe. While pneumonia can sometimes resolve on its own, there are numerous cases that lead to severe complications, including death, such as pneumonia caused by the SARS-CoV-2 virus. Therefore, individuals exhibiting symptoms suggestive of pneumonia should seek medical attention at reputable healthcare centers or hospitals. It is unwise to assume that pneumonia can resolve without treatment or with inadequate treatment, as this can lead to dangerous complications.
8. Is Pneumonia Dangerous?
Pneumonia is a relatively serious condition with many unpredictable complications. In particular, pneumonia caused by the SARS-CoV-2 virus poses a global health threat. The number of deaths from COVID-19 has not shown signs of decreasing. Thus, it is advisable to take proactive measures to prevent pneumonia for yourself and your family by maintaining hygiene, wearing masks, washing hands frequently, and avoiding crowded places while the COVID-19 pandemic remains uncontrolled.
9. Is Pneumonia Curable?
Pneumonia can be completely treated if detected in a timely manner. Treatment methods need to be tailored to the specific symptoms and the progression of the disease. However, in some cases where the disease has progressed significantly, treatment can be quite challenging.
10. Are Pneumonia and Lung Cancer Similar or Different?
Pneumonia and lung cancer share some common symptoms such as cough, chest tightness, fatigue, and loss of appetite. Both conditions commonly present with cough; however, the cough associated with lung cancer tends to be persistent, lasting more than two weeks, and does not improve with antibiotics, especially if it is accompanied by blood, which is a warning sign. Typically, patients with early-stage lung cancer may have vague symptoms, making it easy to confuse with other illnesses. Therefore, patients need to undergo examinations and additional clinical tests for accurate diagnosis.
11. Can Pneumonia Recur?
Currently, it is not uncommon for children to experience recurrent pneumonia multiple times. Recurring pneumonia can lead to severe complications and even death.
12. Can Pneumonia Cause Diarrhea or Back Pain?
Pneumonia can lead to diarrhea and vomiting in both adults and children. Additionally, pneumonia occurs when the thin membrane lining and protecting the lung cavity is severely damaged. This condition can cause sharp pain in the back behind the lungs, possibly accompanied by high fever and cough.