Even if the Covid-19 variant has high transmissibility like Omicron maximizes its “tools,” biochemical laws suggest that the virus cannot evolve indefinitely.
Has Omicron Evolved to Its Maximum Potential?
Whether a virus is alive or not is a contentious issue, but like all forms of life, they evolve. This fact has become increasingly clear during the Covid-19 pandemic, as new variants of concern have emerged every few months.
Some of these variants are more transmissible from person to person and have become the dominant variants by surpassing the slower-evolving versions of the SARS-CoV-2 virus.
This increased transmissibility is believed to be due to mutations in the spike protein, which help the virus bind more tightly to ACE2 receptors. ACE2 receptors are located on the surface of cells, where the virus attaches to enter the human body and begin replicating.
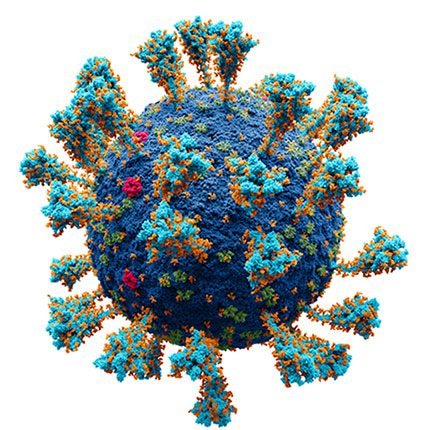
Omicron may be the variant that has reached its maximum transmissibility. (Illustration: Wiki Commons).
These mutations previously allowed the Alpha variant and then the Delta variant to become globally dominant. Scientists predict that a similar situation may occur with the Omicron variant.
However, viruses cannot indefinitely improve their capabilities. Biochemical laws imply that viruses will eventually evolve their spike protein to bind to ACE2 as effectively as possible. Once that threshold is reached, the ability of SARS-CoV-2 to spread between individuals will not be limited by how well the virus can attach to the outer layer of cells.
Nonetheless, other factors will limit the virus’s spread, such as how quickly the genetic material can replicate, how rapidly the virus can enter cells via the TMPRSS2 protein, and how effectively the virus can release from an infected person. In principle, all these characteristics will eventually evolve to their highest potential.
The question arises: has the Omicron variant evolved to its highest potential? There is no reason to assert that it has. Gain-of-function research, which examines what mutations SARS-CoV-2 needs to spread more effectively, has identified several mutations that enhance the spike protein’s ability to bind to human cells, which the Omicron variant lacks.
Nonetheless, it is possible that Omicron is the variant that has reached its maximum transmissibility. Perhaps Omicron will not have any more effective tools as it is limited by its genetic capabilities. This is similar to how zebras will not evolve to have more eyes at the back of their heads to avoid predators. SARS-CoV-2 cannot select mutations to achieve maximum evolutionary potential theoretically, as these mutations need to occur simultaneously, which is impossible.
Even in the scenario where Omicron is the most transmissible variant among humans, new variants will emerge to counteract the human immune system.
After contracting any virus, the immune system adapts by producing antibodies that bind to the virus to neutralize it, and T cells destroy the infected cells. Antibodies are protein fragments that attach to virus molecules, and T cells recognize infected cells by the shape of these molecules. Therefore, SARS-CoV-2 can evade the immune system through variants that alter the shape of these molecules to avoid detection.
This is why Omicron has been so “successful” in infecting those who have previously been infected or vaccinated. Additionally, mutations that enhance the spike protein’s binding to ACE2 also reduce the ability of antibodies to attach to the virus and neutralize it.
The Final Variant of Concern?
Data from Pfizer indicates that T cells respond to the Omicron variant similarly to previous variants. This aligns with observations that Omicron has caused lower mortality rates in South Africa.
What is important for us is that prior infection seems to protect individuals against severe symptoms and the risk of death.
This point may represent the future of this virus. Even if the virus becomes “more professional” and maximizes all its tools, it will still be controlled and eliminated by the immune system. Mutations may enhance transmissibility but will not significantly increase mortality rates.
This virus may achieve maximum evolution and then randomly mutate, changing shape over time to evade immune recognition, thereby causing waves of reinfection. At that point, we might experience a Covid-19 season every winter, similar to the current seasonal flu. Influenza viruses also undergo similar mutations over time, known as “antigenic drift”, leading to reinfection.
New flu viruses each year are not necessarily stronger than those from previous years; they are simply more different. The clearest evidence of the fate of the SARS-CoV-2 virus may be 229E, a coronavirus that causes the common cold.
Thus, Omicron may not be the final variant, but it could be the last variant of concern. If we are lucky, in the unpredictable context of the pandemic, SARS-CoV-2 will become an endemic virus that mutates slowly over time.
This disease may become very mild as those who have previously been infected develop immunity, reducing the risk of hospitalization and death. Most people will contract the virus for the first time in childhood, which may occur before or after vaccination, and thus subsequent reinfections may go largely unnoticed.
At that point, we will only need a small group of scientists to monitor the genetic changes of the SARS-CoV-2 virus over time, and variants of concern may become a thing of the past, at least until the next virus crosses the species barrier.


















































