According to Dr. Hong Zhi Jian (Hồng Chí Kiên), the head of the external orthopedic department and the lead expert on the project “Allograft Tissue Transplantation on the Face” at the Nanjing Military General Hospital, since 2003, China has been preparing for clinical applications and performing facial transplantation surgeries.
Preparing “Materials” for Facial Transplantation
In addition to the transplantation procedure itself, the first issue that needs to be addressed is the “acquisition of materials.” It is necessary to obtain a complete facial skin graft that includes adequate subcutaneous fat, arteries, veins, and even nerves, while ensuring proper blood supply. Currently, this technique is entirely feasible.
 |
Diagram of a facial transplantation surgery conducted by Chinese experts |
Dr. Hong Zhi Jian’s research team has conducted cadaveric surgical studies to identify incision sites and layer dissection, such as which subcutaneous tissues can be removed. The incision will generally be made from the hairline down to the temples and straight down to the chin. During anatomical experiments, they discovered that if the neck skin is involved, it cannot guarantee blood supply.
In the experimental process, the eye skin proved to be the most challenging to handle due to its small, thin structure and critical layering. If the eye skin is too thick after surgery, it will protrude; if too thin, it will not ensure blood supply.
The facial grafting technique requires the complete removal of the donor’s facial skin within 6-8 hours after death.
The research team successfully acquired “materials” from a fresh cadaver within half an hour, with the longer duration allocated for cutting and refining the facial skin tissues after retrieval. Since skin tissues can only endure ischemic conditions for a limited time, it is crucial to complete the vascular anastomosis within 10 hours.
In some other countries, previous experiments have involved facial grafting on animals, such as transplanting the facial skin of a black mouse onto a white mouse, resulting in the white mouse’s fur growing normally. However, this result is only of reference significance, as the facial structure of humans is unique.
Once blood circulation is secured and the skin tissues are viable, restoring the ability to express emotions with the new face becomes a complex challenge.
Facial Reconstruction After Surgery
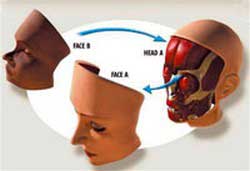 Initially, it depends on the extent of deformation of the patient’s face, followed by the viability of the transplanted skin tissue, which must connect naturally with the remaining skin of the patient.
Initially, it depends on the extent of deformation of the patient’s face, followed by the viability of the transplanted skin tissue, which must connect naturally with the remaining skin of the patient.
If the transplanted facial skin is 5mm thick, after successful surgery and waiting for inflammation to subside, it can restore to normal thickness. If the new skin does not survive well and swells to 15mm, the deep muscle expressions may be hard to achieve because they rely on muscle function. If the entire surgical process goes smoothly, basic expressions such as smiling should not be problematic.
After the surgery, there may be a short-term risk of vascular occlusion causing skin necrosis, a common issue in microsurgical procedures.
Moreover, the face, being an external organ, is prone to infections due to open wounds.
The greatest danger of facial transplantation surgery is the risk of post-operative rejection, a challenge that recipients will face for life.
Within a few days to 1-2 months post-surgery, if there is acute rejection, it can still be managed with medication. However, if chronic rejection occurs, medication may not be effective, and it could lead to tissue necrosis and shedding. This phenomenon can currently only be addressed at the level of corrective surgery if the initial operation fails.
Rejection reactions will necessitate lifelong immunosuppressant therapy, which comes with side effects. Currently, managing these side effects is limited to safety levels that do not threaten the patient’s life.
The new face after surgery will retain 60% of the patient’s original appearance and 40% will reflect the donor’s features. Patients with ordinary burns should not take the risk of undergoing such a major surgery. This surgical method should only be applied to patients with severe burns, those who have been in serious accidents, animal bites, or those with malignant tumors on their face.
Nguyễn Tuyết Nhung