Painkillers are often likened to miracle drugs; without them, doctors would hesitate to perform many complex surgeries.
When a rabbit is injured, it will flatten its ears, squint its eyes, and endure the pain until it subsides. Rabbits do not typically show their pain outwardly, as thrashing on the ground could attract the attention of predators.
However, larger animals, such as horses, do not hide their pain. They will whinny loudly and sometimes thrash about like a child screaming. Science indicates that this behavior can sometimes help alleviate pain a little.
Predatory animals like wolves and lions are often seen licking their wounds. This action may help soothe cut nerve endings, reduce irritation, lessen inflammation, and even speed up their healing process.
In fact, it’s not only mammals that feel pain; birds, reptiles, fish, and mollusks like snails also experience it. Every creature on Earth has its own way of managing pain, but none, except humans, know how to signal for medicine and purchase a pack of paracetamol.
Human painkillers are often regarded as exclusive miracle drugs. They allow us to manage all the suffering in our lives, from a toothache, a severe sore throat, to the necessity of undergoing surgery.
And even the final pains of a cancer patient in palliative care can be eased with painkillers. With medication, everything becomes more bearable.
For instance, this YouTuber would never have been able to undergo a leg-lengthening surgery without pain relief: “When I scream in pain, they prepare some medication, and within 10 seconds, my leg feels no pain at all. It’s truly amazing!“
So, how do painkillers actually work? Why do they have such miraculous effects?

Types of painkillers.
First, let’s talk about pain
In reality, pain is a beneficial response for the body. It signals to us what to do to avoid harming ourselves. Pain tells us to use a hammer more carefully, to eat soup only after it has cooled, and to never touch fire.
There are some people in the world who cannot feel pain. It may sound like a superpower—children pulling out teeth, mothers giving birth without anesthesia. However, the inability to feel pain is classified by doctors as a disability, a condition rather than a desirable ability.
Jo Cameron, a Scottish woman with a condition that prevents her from feeling pain, has described how she has suffered in her life. At the age of 8, Cameron broke her arm without realizing it. She also frequently burned herself and only recognized her burns when she smelled charred flesh.
From an evolutionary standpoint, those who cannot feel pain tend to have shorter lifespans than average. This is because they cannot recognize or protect themselves from environmental threats. Thus, evolution does its selective work, preventing the genes that inhibit pain from being widely inherited.

Jo Cameron, a Scottish woman with a condition that prevents her from feeling pain.
However, the consequence of retaining the “pain feature” is that sometimes we must endure severe pain or chronic pain that leads to overall debilitation.
Thus, on one hand, doctors are trying to find treatments for patients who cannot feel pain. On the other hand, they also need medications that help ordinary people manage their pain when necessary.
To achieve both, we must understand how pain is generated.
The Pain Signal Pathway
For example, when you touch a hot object, your hand will retract almost instantly. This is because all over our skin are countless pain receptors known as “nociceptors“.
Pain receptors are also found in muscles, joints, teeth, and some internal organs. Like other nerve cells, they generate electrical signals, sending information from where they are stimulated to the brain.
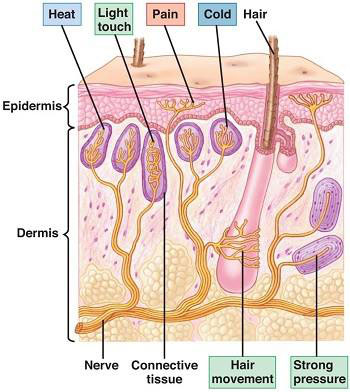
Receptors under the skin detect temperature, pressure, and pain.
However, unlike other nerve cells, nociceptors only send signals when an external event causes damage that exceeds their activation threshold. For example:
When you touch the tip of a needle, your hand also has other tactile receptors that allow you to feel the coldness of the metal and its smooth surface. These tactile receptors continuously transmit signals to your brain.
But the nociceptor has not been activated yet, as the event of touching the needle’s tip has not exceeded its threshold. Only when you gradually press your finger into the needle’s point, to a certain level, will the threshold be broken, and the nociceptor will “turn on.”
It sends out signals, and these electrical signals are captured by nerves and transmitted to the central nervous system in the spinal cord. The process then splits into two pathways: one pathway sends the electrical signal from the spinal cord back to the muscles in the finger, instructing it to retract.
The other pathway sends the signal up the spinal cord to the brain for analysis of the pain you are experiencing. Because the pathway from the spinal cord to the finger is always shorter than the pathway from the spinal cord to the brain, you will retract your hand before you feel pain.
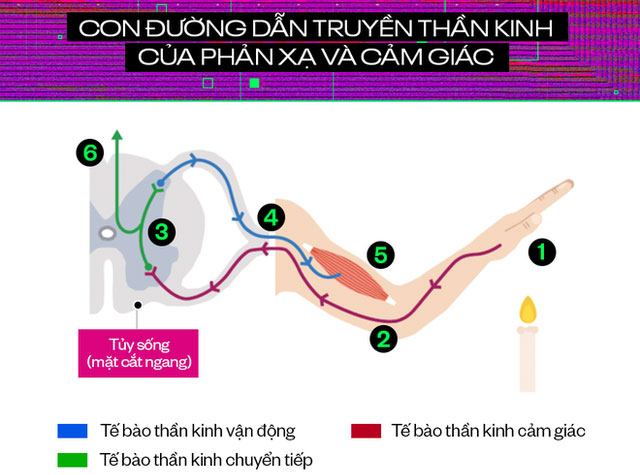
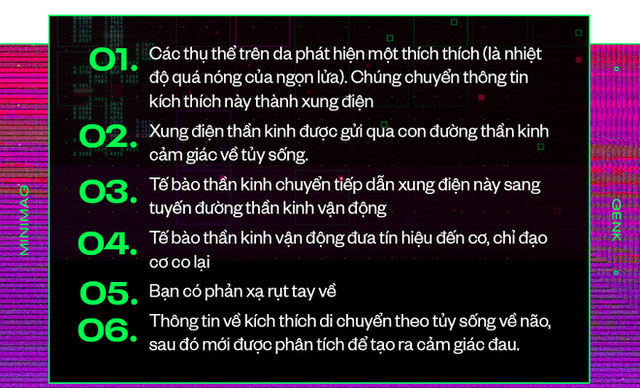
Now, let’s discuss the pain signal. This electrical signal is packaged in the same signal bundle that runs from your finger to the spinal cord. They are generated by cells that come into contact with the damaged tip of the needle.
Cell damage releases arachidonic acid. Arachidonic acid then combines with two enzymes found in the body, COX-1 and COX-2, to be converted into prostaglandin H2.
This substance is then further converted into various other chemicals such as TXA2, PGD2, PGE2, and PGF2. These chemicals create electrical signals that inform the brain to raise body temperature (resulting in fever), trigger an inflammatory response (causing swelling of the injury), and lower the pain threshold of nociceptors.
Once the pain threshold is lowered, nociceptors become very sensitive. You only need to lightly touch the swelling or wound to feel pain. Or some people suffer from chronic pain, with nociceptors being continuously activated.
How Do Painkillers Work?
Once you understand the pain signal pathway and how it is generated, the role of painkillers is simply to choose the right spots to block those pathways, so you will no longer feel pain.
Let’s review how some painkillers do this. First are non-steroidal anti-inflammatory drugs such as ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. All three of these medications block the combination of arachidonic acid with COX-1 and COX-2.
Thus, when damaged cells produce arachidonic acid, it cannot be converted into prostaglandin H2 and other compounds that cause inflammation and lower pain thresholds.
The result is that in the signal package sent from the injury to the brain, there are no longer pain and inflammation signals.
Acetaminophen (Tylenol), also known as paracetamol, has only half the effect. It only blocks the signal packages generated from pain-causing chemicals and does not have anti-inflammatory effects. In contrast, corticosteroid medications like prednisone strongly block inflammatory signals but have little pain-relieving effect.
Next are topical painkillers. They act directly on the nerves near the injury. For example, lidocaine, a local anesthetic, prevents the affected nerves from sending electrical signals, so they cannot travel to the brain and be interpreted as pain.
Another strategy is topical medications that directly target proteins present on nociceptor pain receptors. When these proteins are activated by the medication, they inhibit the nociceptor pain receptors while also creating a distracting sensation, such as a cooling feeling similar to menthol or a warming sensation like that of chili peppers.
These cooling and warming sensations can temporarily interfere with pain signals and make you feel more comfortable. This is also the mechanism of action for various heat or cold ointments, similar to how you might apply ice to an injury.

Topical pain relief sprays are commonly used by football players.
Currently, chronic pain caused by nerve damage, such as in cases of arthritis or diabetic ulcers, can lead to overactive nerves that send pain signals to the brain even in the absence of tissue damage.
The best pain relief medications for these conditions are those that reduce these false alarm signals. For example, gabapentin (Neurontin) is a drug that can inhibit the pain sensation system by blocking electrical signals in the nerves. However, gabapentin can also reduce nerve activity in other parts of the nervous system, potentially leading to drowsiness and confusion.
Antidepressants, such as duloxetine and nortriptyline, may also be effective as they increase certain neurotransmitters in the spinal cord and brain. These neurotransmitters can modulate pain pathways but may also alter chemical signals in the digestive tract, leading to stomach discomfort.
Finally, we turn to a specific type of pain reliever: opioids. The most famous of these opioid pain relievers is morphine, which has been used to treat pain since the 1800s.
In addition to refined morphine, several natural and synthetic derivatives of morphine are also used for pain management, including codeine, tramadol, hydrocodone, oxycodone, buprenorphine, and fentanyl.

Morphine is a pain reliever with a history of over 200 years.
Opioids work by activating the body’s endorphin system. Endorphins are a type of opioid that your body produces naturally, typically creating feelings of euphoria, pain relief, and stress reduction.
Opioid medications like morphine mimic endorphins, acting on receptors in the nerves and brain, blocking the pathway of pain signals, and thus can alleviate certain acute pains such as post-surgical pain, musculoskeletal injuries like fractures, or cancer-related pain.
However, opioids are ineffective for nerve injuries and chronic pain. This type of pain reliever has the side effect of addiction and tolerance decrease. Consequently, each subsequent use requires a higher dose of opioids to achieve the same pain relief effect.
It is evident that while humans have developed many types of pain relievers, each has its own advantages and disadvantages. No current pain reliever can operate perfectly and treat all types of pain simultaneously.
Therefore, the strategy of modern medicine remains to select a suitable medication for a specific type of pain, aiming to cut the pain signal pathway at a particular link.
Meanwhile, scientists are actively researching pain in both humans and animals. Notably, efforts by the International Association for the Study of Pain (IASP), an organization of over 7,200 scientists in 133 countries worldwide, are noteworthy.
In addition to researching and developing new medications, scientists are also continuing to test the effectiveness of various alternative pain relief methods, such as hypnosis, psychological interventions, and acupuncture.
The mechanisms of action on pain signal pathways for these methods may differ from those of chemical drugs. However, regardless of their nature, their ultimate purpose remains to alleviate human suffering. As stated by the IASP, pain relief is also regarded as a human right that everyone should have access to.



















































