A research team at Stanford has invented a strange new molecule that could lead to gene-activating drugs and cause cancer to self-destruct.
All cancers contain molecules that promote uncontrolled growth. What if scientists could link these molecules to others that trigger self-destruction in cells? Could the survival drives of cancer activate its own destruction?
This idea came to Dr. Gerald Crabtree, a developmental biologist at Stanford, during a walk in the redwood forest near his home, and he immediately set out to implement this idea and plan to make it a reality.
In a recent study published in the journal Nature, Dr. Crabtree, along with Nathanael S. Gray, a professor of systems biology and chemistry at Stanford, and several colleagues, reported results they achieved from Dr. Crabtree’s idea. Although developing a drug based on this concept is still a long way off, it has the potential to become a target for drug developers in the future.
Jason Gestwicki, a professor of medicinal chemistry at the University of California, San Francisco, described this idea as brilliant and compared it to turning an essential vitamin into a toxin that kills cancer cells: “It’s brilliant. It transforms something that cancer cells need to survive into something that can kill them, like turning your vitamin into poison.“
Dr. Louis Staudt, director of the Cancer Gene Center at the National Cancer Institute, called this a potential new approach to turn cancer against itself. He expressed interest in conducting clinical trials with patients who have exhausted other treatment options once this method is further developed.
Through laboratory experiments, they used cells from a blood cancer known as diffuse large B-cell lymphoma. The researchers devised molecules that link two proteins together: BCL6, a mutated protein that cancer depends on for robust growth and survival, and a normal protein that activates nearby genes.
This new approach could be an improvement over the challenging task of blocking all BCL6 molecules with drugs. By only rewinding a part of the BCL6 molecules, it could destroy cancer cells.
Dr. Crabtree believes this concept could be effective for half of all cancers, as they involve known mutations that create growth-promoting proteins. Additionally, because the treatment targets mutated proteins specific to cancer cells, it could be highly specific and sparing to healthy cells.
Dr. Crabtree identified two key discoveries that made this work feasible. The first was identifying the “driver genes”—about a few hundred genes that, when mutated, contribute to the spread of cancer. The second was discovering the cell death pathway, used to eliminate bad cells. Each individual has about 60 billion cells affected daily by these pathways.
According to Dr. Staudt, BCL6 is the main regulator of these cancer cells. When its function is completely disrupted, the cell loses its identity and recognizes that something is seriously wrong.
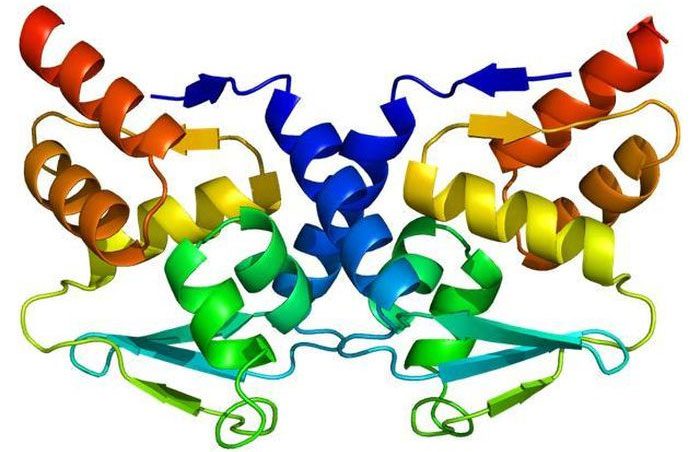
BCL6, a mutated protein that cancer depends on for growth.
The main effect of the experimental treatment, as explained by Dr. Crabtree, is to activate cell death genes. The research team tested the hybrid molecule on mice; however, as Dr. Staudt pointed out, humans are biologically different from mice.
Stuart L. Schreiber, a professor of chemistry and chemical biology at Harvard and a former collaborator of Dr. Crabtree, described this work as “exciting” but cautioned that it is still not a drug and there is a long road ahead.


















































