A series of viruses have re-emerged as the Covid-19 pandemic has subsided in most countries. However, these viruses are behaving unusually.
Unpredictable Virus Behavior
According to CNBC, seasonal flu is one example. The winter season of 2020 and 2021 saw the mildest flu outbreaks, both in terms of deaths and hospitalizations. However, flu cases surged in February and continued to rise in spring and summer as Covid-19 prevention measures were lifted.
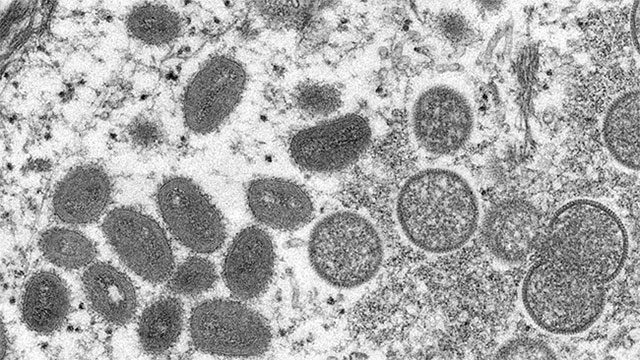
Image of monkeypox virus under an electron microscope.
Dr. Scott Roberts, Deputy Medical Director for Infectious Disease Prevention at Yale New Haven Hospital (USA), told CNBC on June 8: “We have never seen flu season in the U.S. extend into June. Covid-19 has clearly had a major impact on that. Now that people are not wearing masks and many places are reopening, we are seeing viruses behave in very strange ways that we have not seen before.”
Influenza is just the starting example. Next is the Respiratory Syncytial Virus – a common cold virus typically seen in winter months. This virus was notably active last summer, with rising cases among children in Europe, the U.S., and Japan.
Then, in January, an outbreak of Adenovirus 41 – a virus that usually causes gastrointestinal illness – appeared to be a clear cause of serious and mysterious liver disease in young children.
The state of Washington in the U.S. has experienced the worst tuberculosis outbreak in 20 years.

Healthcare workers treating a child with monkeypox in Zomea Kaka, Lobaya region, Central African Republic.
Currently, the recent outbreak of monkeypox, a rare viral infection typically found in Central and West Africa, is challenging healthcare experts with over 1,000 confirmed and suspected cases emerging in 29 non-endemic countries.
The U.S. Centers for Disease Control and Prevention (CDC) reported that at least two genetically distinct monkeypox variants are circulating in the U.S., likely stemming from two separate animal-to-human transmission events.
Last week, the World Health Organization noted that this strain of monkeypox virus may have gone undetected in society for several months or possibly a few years. Mr. Roberts stated: “The two strains may indicate that the transmission process has been ongoing longer than we initially thought.” He noted that the coming weeks will provide insights into the virus, which has an incubation period of 5 to 21 days.
It remains unclear whether the monkeypox-like virus is mutating, although health experts have reported that it is behaving in new and atypical ways. Notably, the virus seems to be spreading within communities – primarily through sexual contact – rather than through typical environments where the virus might circulate.
Symptoms are also presenting unusually. Mr. Roberts mentioned: “Patients are showing different manifestations than what we previously knew.” He noted that some infected individuals do not exhibit initial flu-like symptoms but instead present with rashes and lesions, particularly unusual ones on the genital and anal areas.
He added: “There are many unknowns that concern me. We are seeing very atypical behaviors from some types of viruses.”
Covid-19 Prevention Measures Reduced Exposure and Immunity
One explanation for these phenomena is that Covid-19 prevention measures and mask-wearing habits have made it difficult for other infectious disease viruses to spread in the usual ways.
In places where viruses could bypass these precautions, they are often overlooked because public health surveillance has primarily focused on the Covid-19 pandemic.
This was the case with the tuberculosis outbreak in Washington, where Covid-19 led to undiagnosed tuberculosis cases.
Now, without Covid-19 preventive measures, previously dormant viruses have found a fertile breeding ground in new “socially starved” hosts eager for social interaction and travel.
Last month, a senior advisor to the WHO indicated that the recent monkeypox outbreak is believed to have originated from two large events in Europe.
Meanwhile, two years of reduced contact due to Covid-19 have diminished individual immunity to diseases and made society as a whole more vulnerable, particularly among young children.
Many Children Missed Vaccination Opportunities
Image depicting a virus causing hepatitis.
This could explain the rising cases of acute severe hepatitis in children.
The U.S. Centers for Disease Control and Prevention also expressed concern that lockdowns may have caused many children to miss vaccinations, potentially increasing the risk of other vaccine-preventable diseases such as measles and whooping cough.
Ms. Jennifer Horney, a professor of epidemiology at the University of Delaware, told CNBC: “To prevent these diseases from rising, we need accelerated vaccination campaigns globally.
Avoiding “Bias in Surveillance”
Post-Covid-19, awareness and the process of monitoring public health issues have also been heightened.
Public health systems established to identify Covid-19 have also aided in diagnosing other diseases.
Professor Eyal Leshem, an infectious disease expert at Sheba Medical Center, agrees: “The public and the media have become much more interested in outbreaks of zoonotic diseases and infectious diseases.”
However, he also warns of “bias in surveillance”, whereby individuals and healthcare professionals are more likely to report cases. This may create the impression that certain viruses, such as monkeypox, are on the rise, while previously, few reported these cases.
Mr. Leshem stated: “It’s not that this disease is more common, but rather that it is receiving more attention.”
Nonetheless, enhancing surveillance of infectious disease outbreaks is not a bad thing. As viruses spread and mutate more, understanding the nature of these outbreaks becomes increasingly important.



















































